14.09 Control of Blood Glucose
Importance of Blood Glucose Regulation
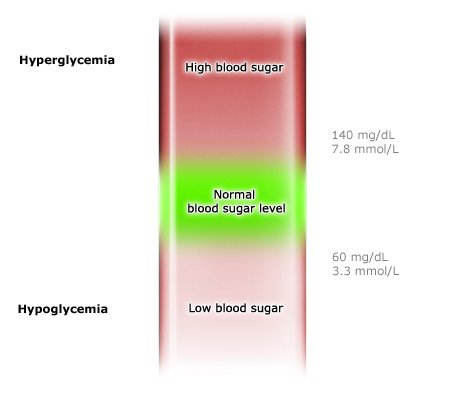
- Normal Range: Blood glucose concentration is generally maintained around 100 mg per 100 cm³ of blood, equivalent to 4.4−6.7 mmol dm⁻³.
- Consequences of Imbalance:
- Hypoglycemia (Low Blood Glucose): Cells, especially brain cells, may not receive enough glucose, risking unconsciousness and cellular damage.
- Hyperglycemia (High Blood Glucose): High glucose concentrations lower the water potential of blood, drawing water out of cells and risking dehydration, which can also lead to unconsciousness.
Key Components of Blood Glucose Control
Pancreas location:
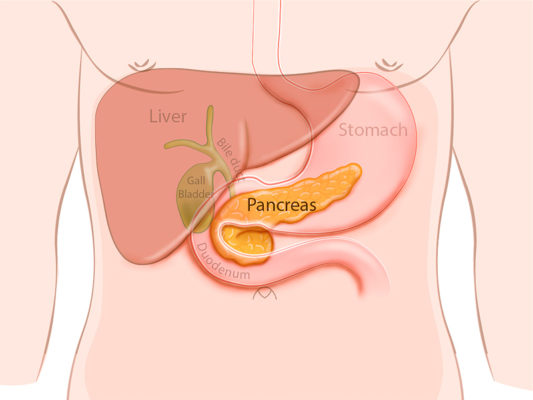
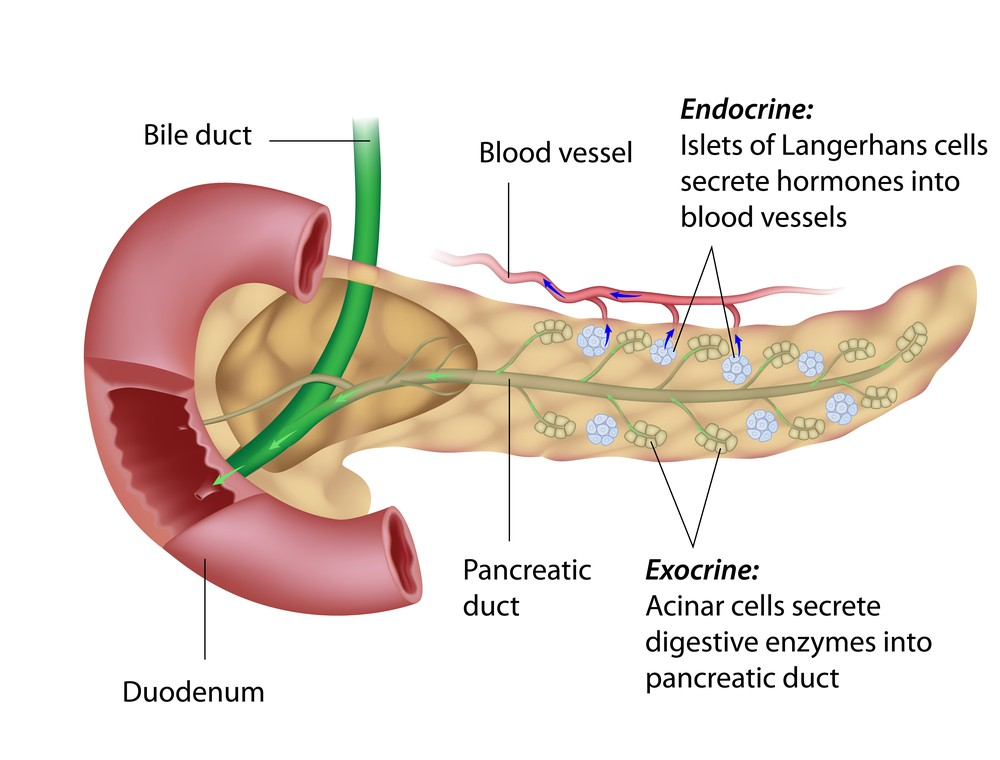
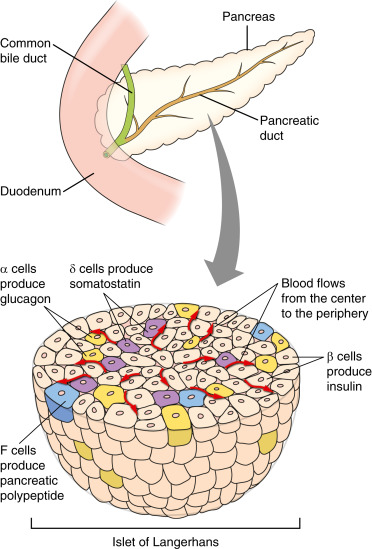
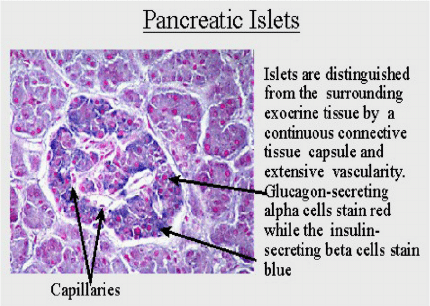
- Pancreas (Islets of Langerhans):
- α Cells: Secrete glucagon to increase blood glucose concentration.
- β Cells: Secrete insulin to decrease blood glucose concentration.
- Islets of Langerhans: Are a cluster of cells (α, β, δ/delta cells) in the pancreas that acts as receptors and control centers in the blood glucose regulation system, releasing insulin or glucagon as necessary.
- Hormones:
- Insulin: Lowers blood glucose by promoting cellular glucose uptake and glycogen synthesis.
- Glucagon: Raises blood glucose by stimulating glycogen breakdown and gluconeogenesis in the liver.
Mechanisms of Blood Glucose Regulation
- When Blood Glucose Increases (e.g., after Eating Carbohydrates):
- Detection: β cells detect the rise in glucose.
- Response:
- Insulin Secretion: β cells release insulin, which circulates through the bloodstream to target cells.
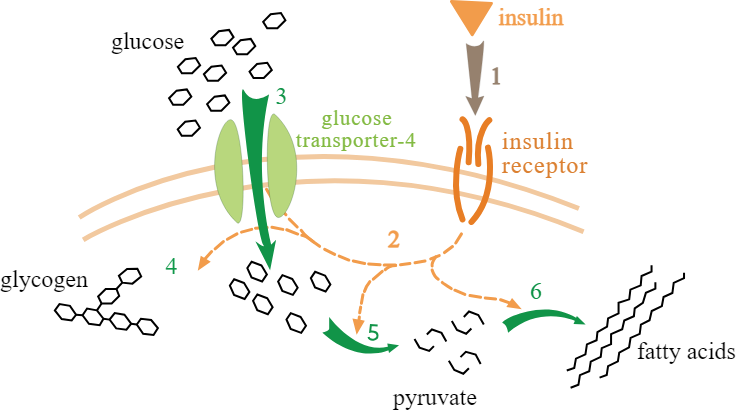
- Insulin Action: Insulin binds to receptors on liver, muscle, and fat cells, promoting glucose uptake and conversion to glycogen (glycogenesis).
- GLUT Transporters: Insulin stimulates the movement of GLUT4 transporters to the cell membrane in muscle cells, enhancing glucose uptake. In liver cells, insulin activates enzymes like glucokinase for glycogen synthesis.
- Outcome: Blood glucose concentration decreases as cells store glucose or use it for energy.
- When Blood Glucose Decreases (e.g., During Fasting or Exercise):
- Detection: α cells detect the drop in glucose.
- Response:
- Glucagon Secretion: α cells release glucagon, which mainly targets liver cells.
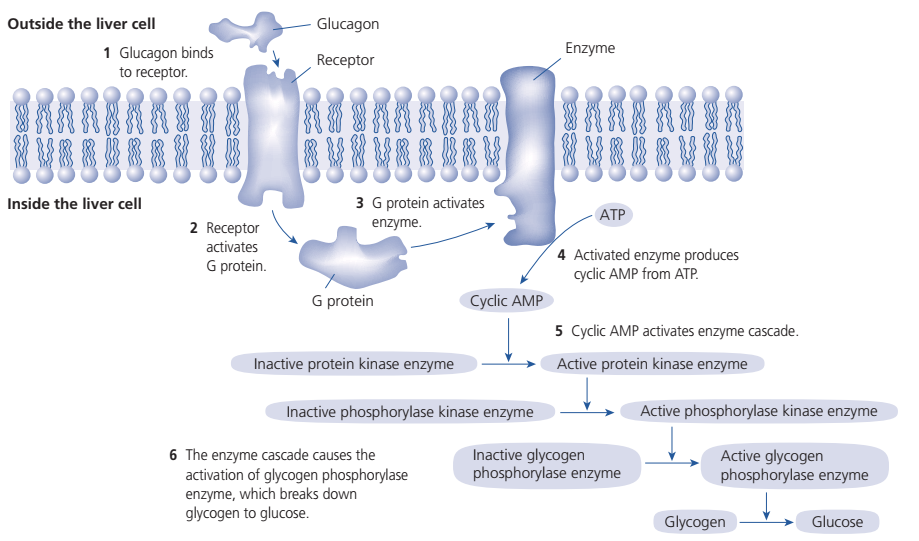
- Glucagon Action: Glucagon binds to liver cell receptors, initiating a signaling cascade (via cAMP) that activates glycogenolysis (glycogen breakdown) and gluconeogenesis (formation of glucose from non-carbohydrate sources).
- Outcome: Glucose is released into the bloodstream, raising blood glucose concentration back toward normal.
Cell Signaling in Insulin and Glucagon Action
- Insulin:
- Insulin binds to specific receptors on target cells, activating a signaling pathway that enables glucose uptake and glycogen formation.
- Signal Transduction: This binding triggers intracellular messengers (e.g., cAMP) and enzymes like phosphofructokinase and glycogen synthase for glycogenesis.
- Glucagon:
- Signaling Cascade: Glucagon binds to liver cell receptors, activating adenylyl cyclase, which converts ATP to cAMP.
- Enzyme Cascade and Amplification: cAMP activates protein kinase A, which in turn activates glycogen phosphorylase to break down glycogen into glucose. Each step amplifies the initial signal, ensuring an efficient response to low blood glucose.
Additional Factors Influencing Blood Glucose
- Adrenaline: Increases blood glucose by promoting glycogen breakdown in the liver and muscle during stress or physical activity, quickly supplying energy.
- Negative Feedback Mechanism: Insulin and glucagon levels adjust in response to glucose fluctuations, keeping blood glucose near a set point despite changes from diet or activity.
Methods of Measuring Blood Glucose

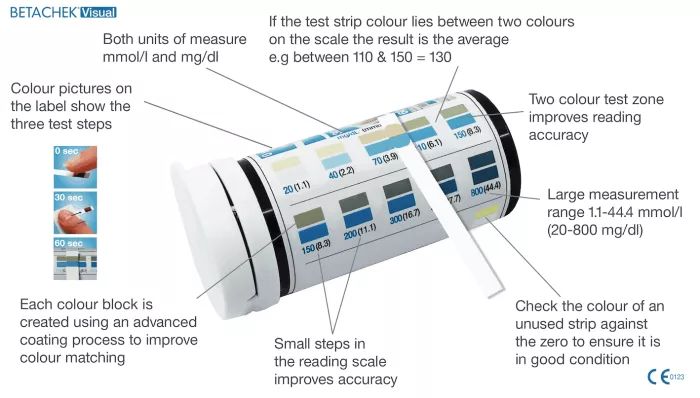
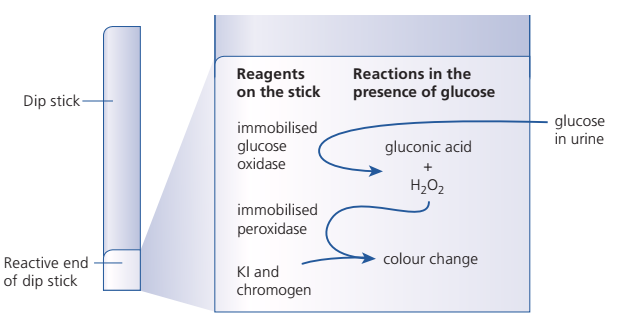
- Urine Testing with Dipsticks:
- Purpose: Detects glucose levels above the renal threshold, indicating potential diabetes.
- Mechanism: Dipsticks contain glucose oxidase and peroxidase enzymes. These react with glucose to produce gluconic acid and hydrogen peroxide, causing a color change that correlates with glucose levels.
- Biosensors for Blood Glucose:
- Purpose: Provides precise, real-time blood glucose levels for diabetes management.
- Mechanism: Contains immobilized glucose oxidase, which reacts with glucose to produce a small electric current proportional to glucose concentration. This current is converted into a digital readout.
Key Terms
- Glycogenesis: The synthesis of glycogen from glucose.
- Glycogenolysis: The breakdown of glycogen into glucose.
- Gluconeogenesis: The formation of glucose from non-carbohydrate sources.
- Adenylyl Cyclase: Enzyme that produces cAMP.
- cAMP: A second messenger that amplifies the signal from glucagon for rapid glycogen breakdown.
Questions for Understanding
Biosensors provide real-time, precise readings of blood glucose, essential for accurate diabetes management, while dipsticks only measure glucose presence in urine over time.
Components in Blood Glucose Regulation:
- Stimuli: Blood glucose fluctuations.
- Receptors: α and β cells in the islets of Langerhans.
- Effectors: Liver, muscle, and fat cells.
Why is Signal Amplification Important in Glucagon Signaling?
- Amplification ensures an effective response to low glucose levels by rapidly activating enzymes to release glucose.
Advantages of Biosensors Over Dipsticks:
Biosensors provide real-time, precise readings of blood glucose, essential for accurate diabetes management, while dipsticks only measure glucose presence in urine over time.