8.05 Blood
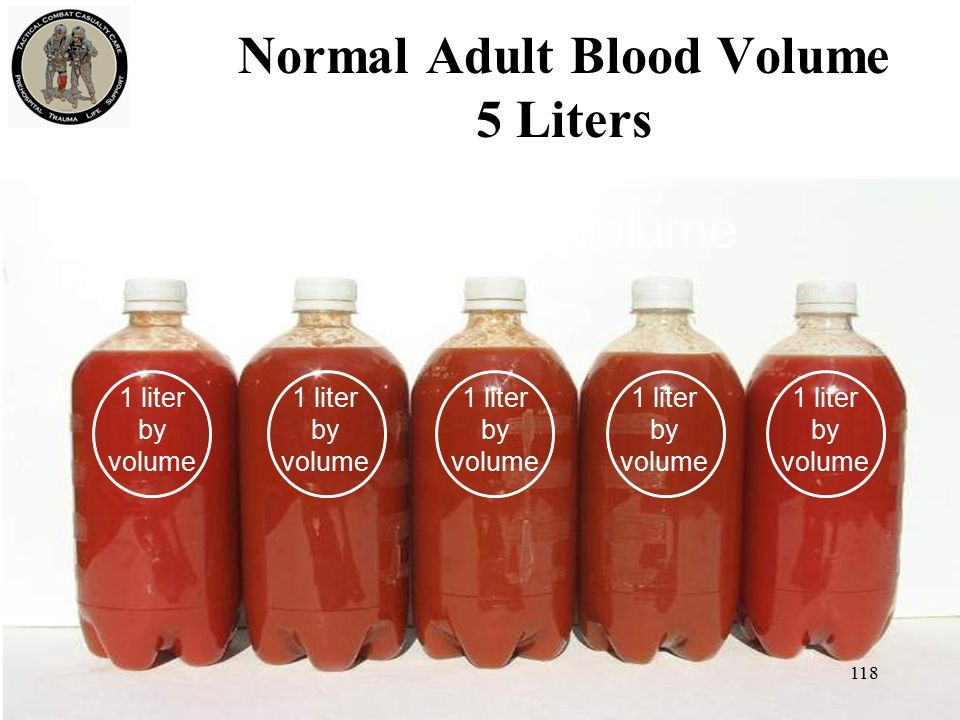
Volume and Mass
- Average Adult Blood Volume:
- Quantity: Approximately 5 dm³ (5 liters) of blood.
- Mass: Roughly 5 kg, considering that blood density is similar to water.
Blood Plasma
Properties
- Composition:
- Water Content: ~95% water, serving as the medium for transporting substances.
- Solutes: Includes glucose, urea, electrolytes, hormones, and other small molecules.
- Functional Attributes:
- Heat Capacity:
- High Heat Capacity: Plasma absorbs and distributes heat throughout the body, aiding in regulating body temperature.
- Heat Capacity:
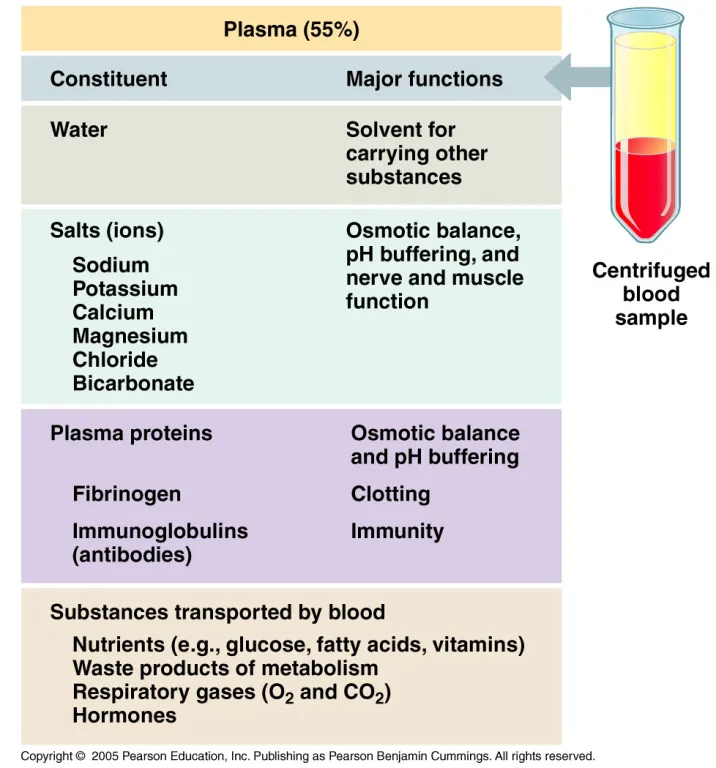
Components
- Solutes:
- Examples: Glucose, urea (a byproduct of protein breakdown in the liver), electrolytes (e.g., sodium, potassium).
- Function: Transport substances between different parts of the body, providing necessary nutrients to cells and removing waste products.
- Plasma Proteins:
- Types:
- Albumin: Maintains osmotic pressure and transports various molecules.
- Globulins: Involved in immune responses (e.g., antibodies).
- Fibrinogen: Essential for blood clotting.
- Origin: Primarily synthesized in the liver.
- Function: Remain within the blood, contributing to blood volume, pressure, and various physiological functions.
- Types:
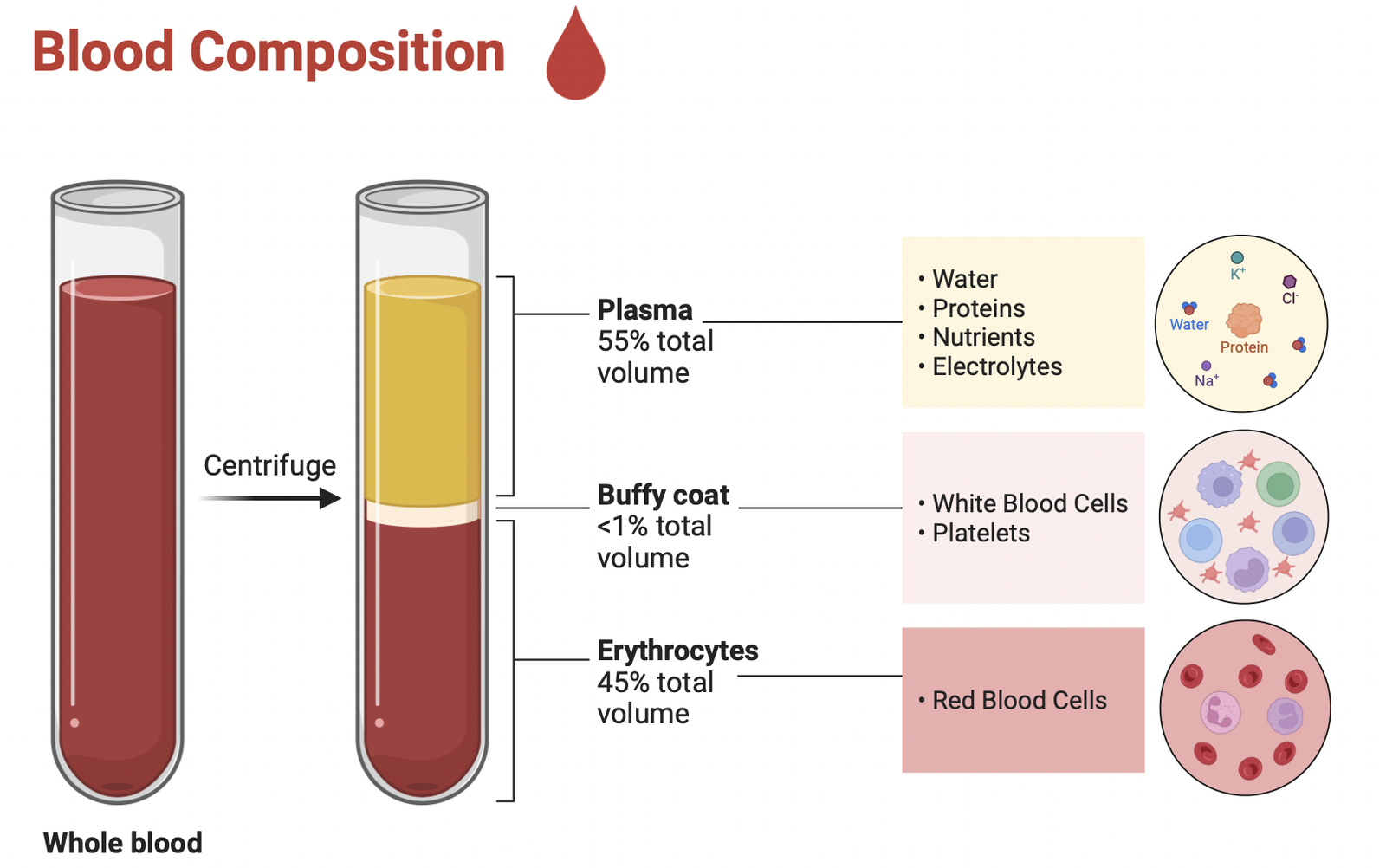
Cell Components in Blood
A) Red Blood Cells (RBCs)
- Quantity: ~2.5 × 10¹³ cells in an average adult.
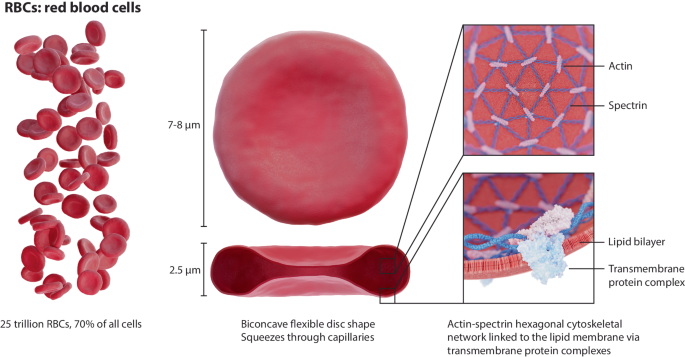
Structure
- Biconcave Disc Shape:
- Purpose: Increases surface area-to-volume ratio for rapid oxygen diffusion.
- Size:
- Diameter: Approximately 7 µm, allowing them to pass through narrow capillaries.
- Flexibility:
- Adaptable Shape: Enables movement through tight spaces in capillaries; supported by the cytoskeleton to retain shape.
- Lack of Nucleus and Organelles:
- Increased flexibility: Helps RBCs squeeze through narrow capillaries.
- Maximum hemoglobin storage: Enhances oxygen-carrying capacity.
Function
- Oxygen Transport:
- Hemoglobin Binding: Hemoglobin molecules bind oxygen in the lungs and release it to tissues.
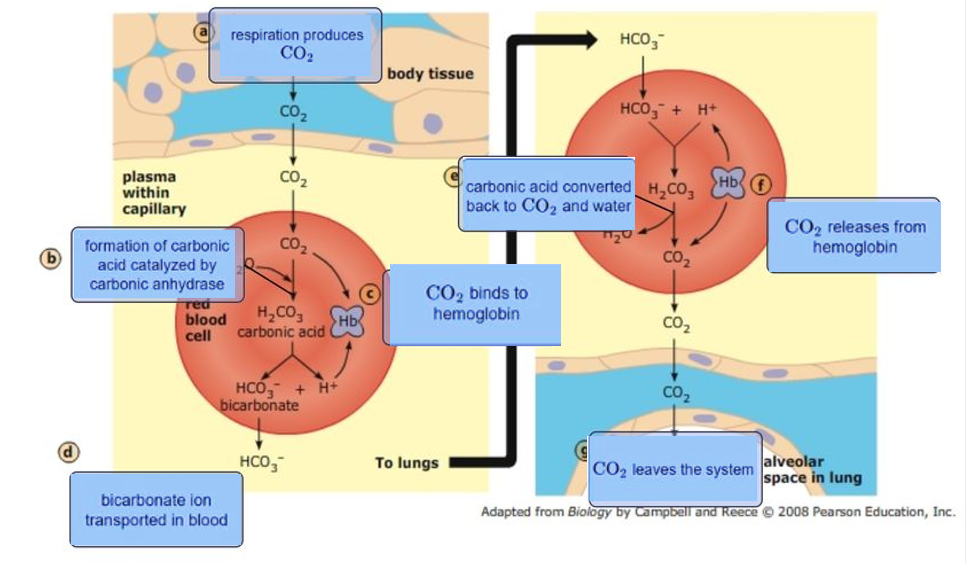
- Carbon Dioxide Transport:
- Secondary Role: Carries carbon dioxide back to the lungs for exhalation.
- Lifespan:
- Duration: Approximately 120 days.
- Removal: Old RBCs are broken down in the liver, with continuous production in the bone marrow.
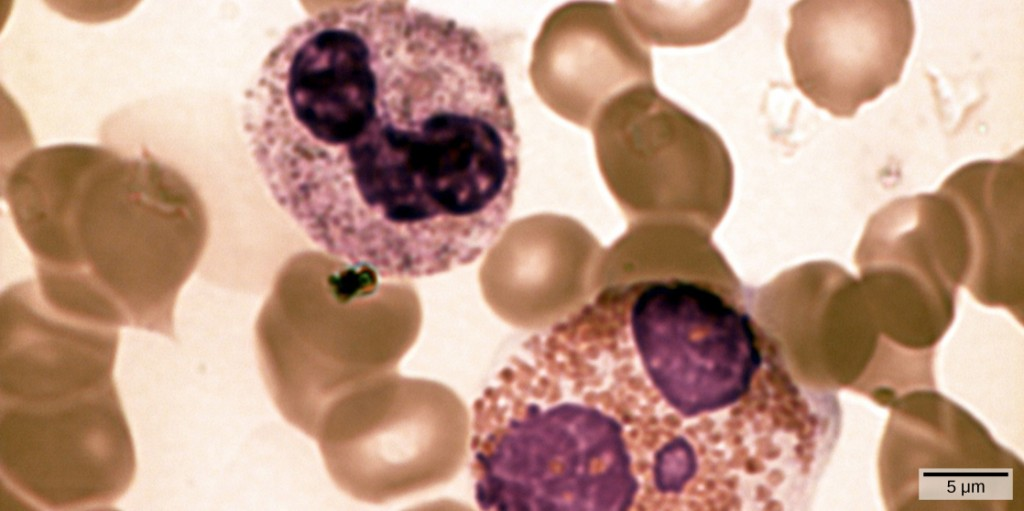
B) White Blood Cells (WBCs)

1. Granulocytes
- Definition: WBCs with visible granules, involved in rapid immune responses.
- Types:
- Neutrophils:
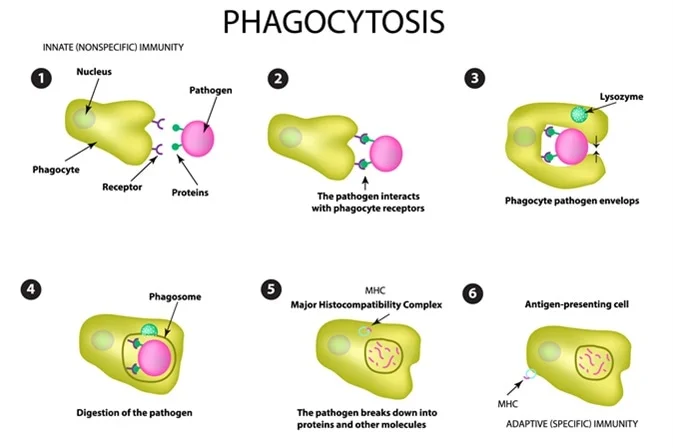
- Function: First line of defense; engulf and destroy bacteria and debris via phagocytosis.
- Cellular Characteristic: Multi-lobed nucleus (2–5 lobes); pale-staining granules.
- Phagocytic? Yes.
- Eosinophils:
- Function: Attack parasites and mediate allergic responses by releasing toxic granules.
- Cellular Characteristic: Bi-lobed nucleus; granules stain red/orange with eosin dye.
- Phagocytic? Mildly phagocytic, mainly for antigen-antibody complexes.
- Basophils:
- Function: Release histamine and mediate inflammation and allergic reactions.
- Cellular Characteristic: Bi-lobed or S-shaped nucleus; dark purple granules obscure the nucleus.
- Phagocytic? No.
- Neutrophils:
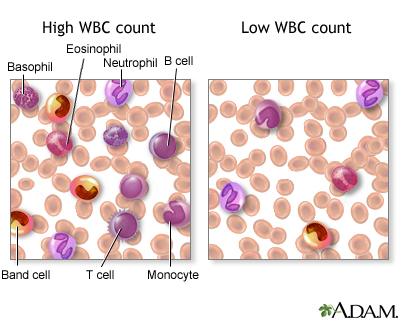

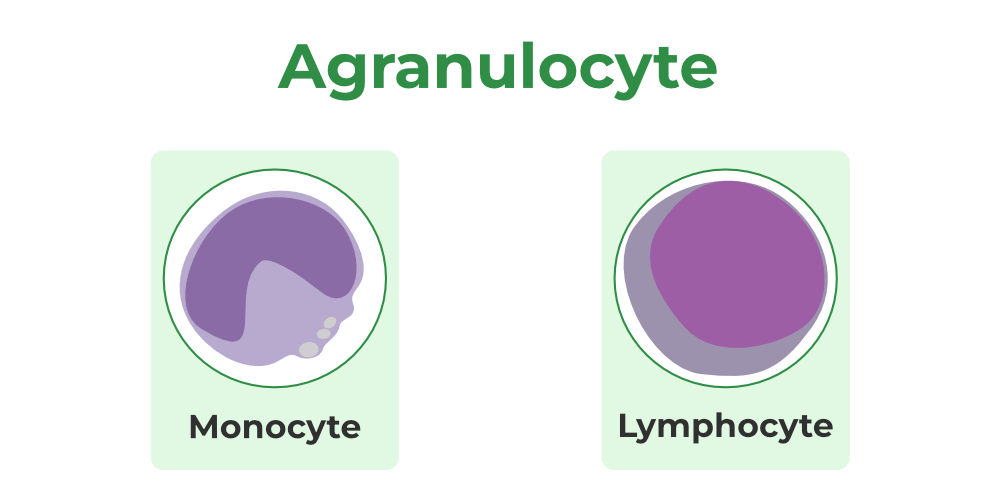
2. Agranulocytes
- Definition: WBCs without visible granules, involved in adaptive and long-term immunity.
- Types:
- Lymphocytes:
- Function: Adaptive immunity (targeted).
- T cells: Kill infected cells and regulate the immune response.
- B cells: Produce antibodies.
- Natural Killer cells: Destroy virus-infected or cancerous cells.
- Cellular Characteristic: Large, round nucleus occupying most of the cell; scant cytoplasm.
- Phagocytic? No.
- Function: Adaptive immunity (targeted).
- Monocytes:
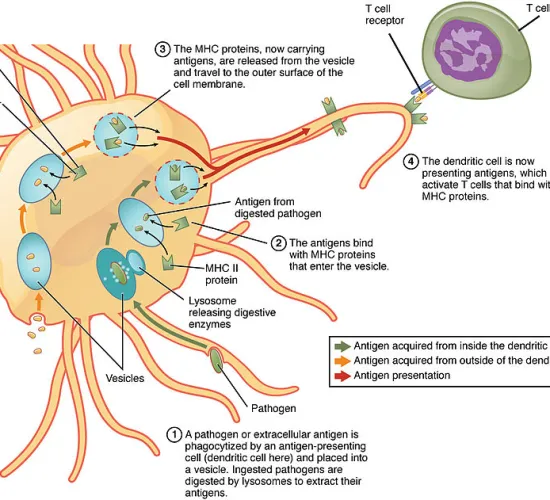
- Function: Phagocytosis and antigen presentation; differentiate into macrophages or dendritic cells in tissues.
- Cellular Characteristic: Large kidney-shaped or U-shaped nucleus; abundant pale cytoplasm.
- Phagocytic? Yes.
- Lymphocytes:
Macrophages (Derived from Monocytes)
- Function:
- Engulf and digest pathogens, dead cells, and debris.
- Present antigens to T cells to activate the immune response.
- Cellular Characteristic: Larger than monocytes, highly dynamic with cytoplasmic extensions for phagocytosis.
- Phagocytic? Yes. Highly efficient.
Phagocytic Cells
- Neutrophils: Primary phagocytic cells; first responders to infections.
- Monocytes: Phagocytic in blood and precursor to macrophages.
- Macrophages: Most versatile and efficient phagocytic cells in tissues.
- Dendritic Cells (derived from monocytes): Specialized in antigen presentation after phagocytosis.
- Eosinophils: Mildly phagocytic, targeting antigen-antibody complexes.
Key Terms
- Plasma:
- The liquid component of blood that transports solutes such as nutrients, hormones, and waste products.
- Plasma Proteins:
- Proteins dissolved in plasma, essential for maintaining osmotic balance, immune functions, and blood clotting.
- Neutrophil:
- A phagocytic WBC with a lobed nucleus and granular cytoplasm; ingests and destroys microbes.
- Monocyte:
- A large WBC with a bean-shaped nucleus; can differentiate into macrophages to phagocytize pathogens.
- Macrophage:
- A phagocytic cell in tissues; engulfs pathogens and presents antigens to lymphocytes to initiate immune responses.
- Lymphocyte:
- A WBC that targets pathogens by producing antibodies (B-lymphocytes) and regulating immune responses (T-lymphocytes).
Practice Questions
Question 1
State the average blood volume and mass in an adult human. (2 marks)
Mark Scheme:
- Blood Volume:
- Approximately 5 dm³ (5 liters) of blood in an average adult. (1 mark)
- Blood Mass:
- Roughly 5 kg, considering blood density is similar to water. (1 mark)
Question 2
Describe the composition of blood plasma and its functional attributes. (5 marks)
Mark Scheme:
- Water Content:
- Blood plasma is composed of about 95% water, serving as the medium for transporting substances. (1 mark)
- Solutes:
- Includes glucose, urea, electrolytes (e.g., sodium, potassium), hormones, and other small molecules. (1 mark)
- Heat Capacity:
- High heat capacity allows plasma to absorb and distribute heat throughout the body, aiding in regulating body temperature. (1 mark)
- Transport Functions:
- Transports nutrients, hormones, waste products, and other substances between different parts of the body. (1 mark)
- Plasma Proteins:
- Includes proteins like albumin, globulins, and fibrinogen, which play roles in maintaining osmotic pressure, immune responses, and blood clotting. (1 mark)
Question 3
List and briefly describe the types of plasma proteins and their functions. (6 marks)
Mark Scheme:
- Albumin:
- Function: Maintains osmotic pressure and transports various molecules such as fatty acids and hormones. (1 mark)
- Globulins:
- Function: Involved in immune responses; includes antibodies that defend against pathogens. (1 mark)
- Fibrinogen:
- Function: Essential for blood clotting, facilitating the formation of a fibrin clot to prevent excessive bleeding. (1 mark)
- Synthesis Origin:
- Primarily synthesized in the liver. (1 mark)
- Other Plasma Proteins:
- May include transport proteins (e.g., transferrin) and enzymes involved in various metabolic processes. (1 mark)
- Overall Role:
- Plasma proteins remain within the blood, contributing to blood volume, pressure, and various physiological functions. (1 mark)
Question 4
Compare red blood cells (RBCs) and white blood cells (WBCs) in terms of structure and function. (6 marks)
Mark Scheme:
- Quantity:
- RBCs: Approximately 2.5 × 10¹³ cells in an average adult.
- WBCs: Approximately 5 × 10¹¹ cells in an average adult. (1 mark)
- Structure of RBCs:
- Shape: Biconcave disc, increasing surface area for gas exchange.
- Size: Diameter of approximately 7 µm.
- Flexibility: Adaptable shape to move through narrow capillaries.
- Lack of Nucleus and Organelles: Maximizes space for haemoglobin. (2 marks)
- Function of RBCs:
- Oxygen Transport: Carry oxygen bound to haemoglobin from the lungs to tissues.
- Carbon Dioxide Transport: Carry carbon dioxide back to the lungs for exhalation. (1 mark)
- Structure of WBCs:
- Nucleus: Present, with varying shapes depending on the type (e.g., lobed for neutrophils, round for lymphocytes).
- Size: Generally larger than RBCs. (1 mark)
- Function of WBCs:
- Immune Responses: Defend the body against infections and foreign invaders.
- Types: Include phagocytes (e.g., neutrophils, monocytes) and lymphocytes (e.g., B-cells, T-cells). (1 mark)
- Overall Comparison:
- RBCs are specialized for gas transport, while WBCs are specialized for immune defense. (1 mark)
Question 5
Explain the role of haemoglobin in oxygen transport and describe its structure. (5 marks)
Mark Scheme:
- Haemoglobin Structure:
- Composed of four polypeptide chains, each containing one haem group that can bind one O₂ molecule. (1 mark)
- Oxygen Binding Capacity:
- Each haemoglobin molecule can bind up to four O₂ molecules (Hb + 4O₂ → HbO₄), allowing efficient oxygen transport. (1 mark)
- Oxygen Transport Function:
- Transports oxygen from the lungs to body tissues for aerobic respiration. (1 mark)
- Cooperative Binding:
- Binding of one O₂ molecule changes haemoglobin’s shape, making it easier for additional O₂ molecules to bind, enhancing overall oxygen uptake. (1 mark)
- Role in Carbon Dioxide Transport:
- Also assists in the transport of carbon dioxide from tissues to the lungs, although RBCs play a secondary role in this process. (1 mark)
Question 6
Define partial pressure and percentage saturation in the context of haemoglobin and gas transport. (4 marks)
Mark Scheme:
- Partial Pressure:
- A measure of the concentration of a gas in a mixture of gases, indicating how much of that gas is available for diffusion. (2 marks)
- Percentage Saturation:
- The percentage of haemoglobin molecules that are bound with oxygen, representing haemoglobin’s capacity to carry oxygen at a given partial pressure. (2 marks)
Question 7
Describe the key features of the haemoglobin dissociation curve and their physiological significance. (6 marks)
Mark Scheme:
- S-Shaped Curve:
- The haemoglobin dissociation curve is S-shaped (sigmoidal), indicating cooperative binding of oxygen. (1 mark)
- Low Oxygen Partial Pressure:
- At low pO₂ (e.g., in tissues), haemoglobin has low saturation, releasing oxygen where it is needed. (1 mark)
- High Oxygen Partial Pressure:
- At high pO₂ (e.g., in lungs), haemoglobin approaches full saturation (95-97%), effectively binding oxygen. (1 mark)
- Cooperative Binding:
- Binding of one O₂ molecule increases haemoglobin’s affinity for additional O₂ molecules, resulting in the steep rise in the curve. (1 mark)
- Bohr Shift Impact:
- Under high CO₂ conditions, the curve shifts right, reducing haemoglobin’s affinity for O₂ and enhancing oxygen release in tissues. (1 mark)
- Physiological Relevance:
- The dissociation curve illustrates how haemoglobin efficiently binds oxygen in the lungs and releases oxygen in tissues, ensuring effective gas transport based on varying oxygen needs. (1 mark)
Question 8
Explain how carbon dioxide is transported in the blood and the role of the chloride shift in this process. (6 marks)
Mark Scheme:
- As Hydrogencarbonate Ions (HCO₃⁻):
- 85% of CO₂ is converted to HCO₃⁻ ions in red blood cells via the enzyme carbonic anhydrase. (1 mark)
- Chloride Shift: HCO₃⁻ ions diffuse out of red blood cells into plasma, while Cl⁻ ions enter red blood cells to maintain ionic balance. (1 mark)
- Dissolved CO₂ in Plasma:
- 5% of CO₂ remains as dissolved molecules in blood plasma. (1 mark)
- As Carbaminohaemoglobin:
- 10% of CO₂ binds directly to haemoglobin, forming carbaminohaemoglobin. (1 mark)
- Reverse Reaction in Lungs:
- In the lungs, the lower CO₂ concentration drives the reverse reaction, releasing CO₂ from HCO₃⁻ ions and carbaminohaemoglobin for exhalation. (1 mark)
- Role of Chloride Shift:
- Maintains ionic balance by exchanging Cl⁻ ions for HCO₃⁻ ions, ensuring blood remains electrically neutral during CO₂ transport. (1 mark)
- Overall Transport Mechanism:
- Ensures efficient removal of CO₂ from tissues and its transport to the lungs for exhalation. (1 mark)
Question 9
Identify and explain two common errors students might make when understanding haemoglobin’s role in gas transport. (4 marks)
Mark Scheme:
- Oxyhaemoglobin Release:
- Incorrect: Oxyhaemoglobin gradually releases O₂ as it passes from the lungs to a muscle.
- Correct Explanation: O₂ is primarily released in tissues where the partial pressure of O₂ is low, not simply based on distance. (2 marks)
- CO₂ Transport:
- Incorrect: Most CO₂ is transported in plasma solution.
- Correct Explanation: Most CO₂ is transported as HCO₃⁻ ions, not dissolved directly in plasma. (2 marks)
Question 10
Describe how the structure of red blood cells enhances their function in gas exchange. (5 marks)
Mark Scheme:
- Biconcave Shape:
- Red blood cells have a biconcave shape, increasing their surface area-to-volume ratio for rapid oxygen diffusion. (1 mark)
- Size:
- Diameter: Approximately 7 µm, allowing them to pass through narrow capillaries. (1 mark)
- Flexibility:
- Adaptable Shape: Enables movement through tight spaces in capillaries; supported by the cytoskeleton to retain shape. (1 mark)
- Lack of Nucleus and Organelles:
- Maximizes Space for Haemoglobin: No nucleus, mitochondria, or endoplasmic reticulum, allowing more haemoglobin molecules for oxygen transport. (1 mark)
- High Haemoglobin Content:
- Rich in haemoglobin, RBCs can carry a large amount of oxygen bound to haemoglobin molecules. (1 mark)