8.04 Tissue Fluid & Lymph

Blood Composition
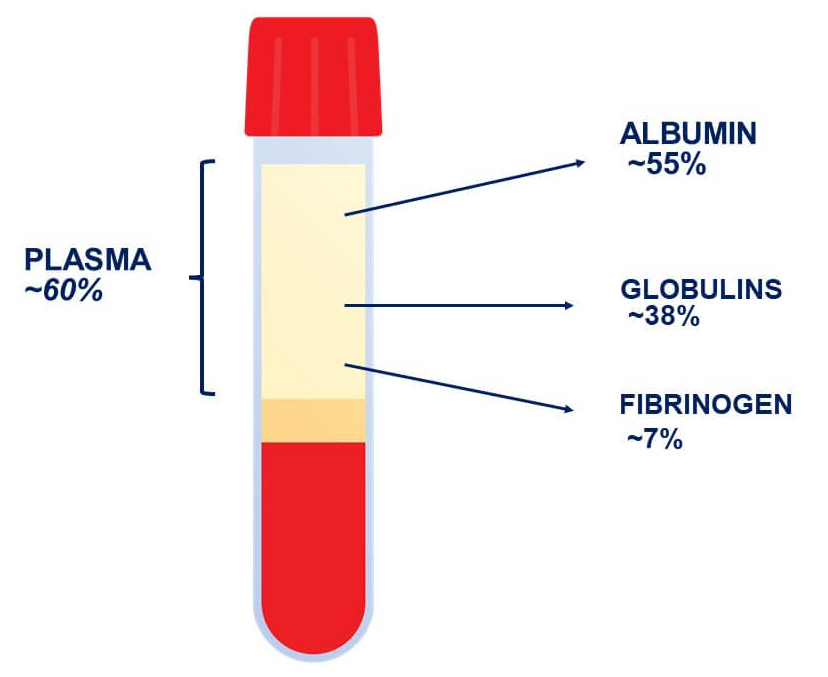
Plasma
- Description:
- Appearance: Pale yellow liquid.
- Main Component: Primarily water (about 90%).
- Contents:
- Solutes:
- Examples: Glucose, urea, electrolytes (e.g., sodium, potassium, calcium).
- Function: Transport substances to and from cells.
- Plasma Proteins:
- Types:
- Albumin: Maintains osmotic pressure and transports hormones, vitamins, and drugs.
- Globulins: Involved in immune responses (antibodies).
- Fibrinogen: Essential for blood clotting.
- Origin: Mainly produced in the liver.
- Function: Remain within the blood, contributing to blood volume and pressure.
- Types:
- Solutes:
- Key Terms:
- Plasma: The liquid component of blood that transports cells, nutrients, hormones, waste products, and other substances.
- Plasma Proteins: Proteins dissolved in plasma, primarily synthesized by the liver, crucial for maintaining blood’s properties and functions.
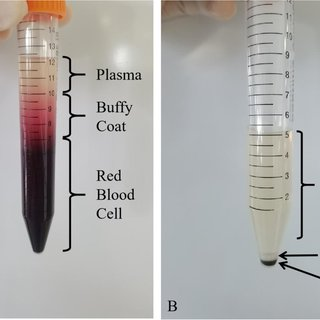
Formation of Tissue Fluid
Tissue Fluid
- Definition: Fluid that has leaked out of capillaries into the spaces between cells.
- Composition:
- Similar to Plasma: Contains water, ions, and small molecules.
- Excludes:
- Large Proteins: Such as albumin, which remain in the blood.
- Red Blood Cells: Do not pass into tissue fluid.
- Cell Movement:
- White Blood Cells (WBCs): Some WBCs can move through capillaries into tissue fluid to perform immune functions.

Movement of Fluid in Capillaries
Capillary Fluid Dynamics
- Arterial End (Capillary Entry)
- High Blood Pressure: Forces fluid out of capillaries into surrounding tissues.
- Water Potential Gradient:
- Higher Protein Concentration in Blood: Creates an osmotic gradient pulling some water back into the capillaries.
- Net Movement: Overall, more fluid moves into tissue fluid at the arterial end.
- Venule End (Capillary Exit)
- Lower Blood Pressure: Reduces the force pushing fluid out.
- Water Potential Gradient:
- Continued Osmotic Pull from Blood Proteins: Encourages water to move back into capillaries from tissue fluid.
- Net Movement: More fluid is reabsorbed into the blood at the venule end.
- Overall Effect:
- Slight Net Fluid Loss from Capillaries: Balanced by the lymphatic system, which drains excess tissue fluid to prevent fluid buildup (edema).


Lymph
Formation of Lymph
1.Entry into Lymphatic Vessels
- A fraction (around 10%) of the interstitial fluid enters blind-ended lymphatic capillaries, which are permeable enough to allow fluid, proteins, and even cells to enter.
- Once the interstitial fluid enters these vessels, it is called lymph.

2. Composition of Lymph
- Similar to plasma but with fewer proteins.
- Can contain white blood cells, especially lymphocytes, and sometimes pathogens, cellular debris, or cancer cells (which is why lymph nodes monitor/filter it).

Lymphatic Circulation
- Lymphatic Vessels
- Lymphatic capillaries merge into larger lymphatic vessels.
- These vessels have one-way valves preventing backflow. Lymph moves slowly, aided by:
- Skeletal muscle contractions (muscular pump)
- Breathing movements (respiratory pump)
- Smooth muscle in larger lymphatic vessel walls
- Lymph Nodes
- Scattered along lymphatic vessels, lymph nodes act as filters.
- Immune cells (e.g., lymphocytes, macrophages) inside nodes detect and fight pathogens.

Return to the Heart
Venous System
- Lymph ducts eventually flows into the superior vena cava (ie., the blood and lymph mixes), then back to the right atrium of the heart.

Continuous Circulation
- This process maintains fluid balance (prevents edema) and allows lymph to be constantly surveyed by immune cells before re-entering circulation.
Conditions and Homeostasis
Oedema
- Definition: Accumulation of excess fluid in tissues, leading to swelling.
- Causes:
- Excess Fluid Leakage: Can occur due to high blood pressure or damage to capillary walls.
- Prevention:
- Role of Arterioles: Arterioles regulate blood flow into capillaries, reducing pressure and minimizing fluid leakage.



Homeostasis
- Definition: Maintenance of a stable internal environment within the body.
- Tissue Fluid Environment:
- Must Remain Constant: Optimal levels of glucose, pH, waste removal, and temperature are essential for proper cell function.
- Regulatory Mechanisms:
- Blood-Brain Barrier, Kidney Function, Hormonal Control: Ensure stable internal conditions despite external changes.
Important Concepts
Permeability of Capillary Walls
- Selective Permeability:
- Small Molecules (e.g., Water, Ions): Pass through capillary walls easily.
- Large Molecules (e.g., Albumin): Rarely pass through, remaining in the blood plasma.
- Relationship with Molecular Mass:
- Smaller Molecules: Higher permeability (e.g., Water with Relative Molecular Mass [RMM] 18, Permeability 1.00).
- Larger Molecules: Lower permeability (e.g., Albumin with RMM 69,000, Permeability 0.00001).
Clinical Relevance
Albumin’s Importance:
- Function: Maintains blood osmotic balance, preventing excessive fluid loss from capillaries into tissues.
- Clinical Significance: Low levels can lead to fluid imbalances and swelling.

Kwashiorkor:
- Definition: A severe form of malnutrition caused by protein deficiency.
- Effects:
- Low Plasma Protein Levels: Reduced albumin lowers blood osmotic pressure.
- Fluid Buildup: Causes tissue fluid to accumulate in tissues, leading to swelling (edema).

Practice Questions
Question 1
State the average blood volume and mass in an adult human. (2 marks)
Mark Scheme:
- Blood Volume:
- Approximately 5 dm³ (5 liters) of blood in an average adult. (1 mark)
- Blood Mass:
- Roughly 5 kg, considering blood density is similar to water. (1 mark)
Question 2
Describe the composition of blood plasma and its functional attributes. (5 marks)
Mark Scheme:
- Appearance:
- Pale yellow liquid. (1 mark)
- Main Component:
- Primarily water (about 90%). (1 mark)
- Solutes:
- Includes glucose, urea, electrolytes (e.g., sodium, potassium, calcium). (1 mark)
- Plasma Proteins:
- Types include albumin, globulins, and fibrinogen. (1 mark)
- Functional Attributes:
- High heat capacity: Absorbs and distributes heat throughout the body, aiding in regulating body temperature. (1 mark)
Question 3
List and briefly describe the types of plasma proteins and their functions. (6 marks)
Mark Scheme:
- Albumin:
- Function: Maintains osmotic pressure and transports hormones, vitamins, and drugs. (1 mark)
- Globulins:
- Function: Involved in immune responses; includes antibodies. (1 mark)
- Fibrinogen:
- Function: Essential for blood clotting, facilitating the formation of a fibrin clot. (1 mark)
- Origin:
- Mainly produced in the liver. (1 mark)
- Other Plasma Proteins:
- May include transport proteins (e.g., transferrin) and enzymes involved in various metabolic processes. (1 mark)
- Overall Role:
- Remain within the blood, contributing to blood volume and pressure. (1 mark)
Question 4
Define tissue fluid and describe its composition. (4 marks)
Mark Scheme:
- Definition:
- Tissue fluid is the fluid that has leaked out of capillaries into the spaces between cells. (1 mark)
- Similar Composition to Plasma:
- Contains water, ions, and small molecules. (1 mark)
- Excludes Large Proteins:
- Does not contain large proteins such as albumin, which remain in the blood. (1 mark)
- Excludes Red Blood Cells:
- Red blood cells do not pass into tissue fluid. (1 mark)
Question 5
Explain how fluid moves in and out of capillaries at the arterial and venule ends. (6 marks)
Mark Scheme:
- Arterial End (Capillary Entry):
- High Blood Pressure: Forces fluid out of capillaries into surrounding tissues. (1 mark)
- Water Potential Gradient: Higher protein concentration in blood creates an osmotic gradient pulling some water back into capillaries. (1 mark)
- Net Movement: Overall, more fluid moves into tissue fluid at the arterial end. (1 mark)
- Venule End (Capillary Exit):
- Lower Blood Pressure: Reduces the force pushing fluid out. (1 mark)
- Water Potential Gradient: Continued osmotic pull from blood proteins encourages water to move back into capillaries from tissue fluid. (1 mark)
- Net Movement: More fluid is reabsorbed into blood at the venule end. (1 mark)
Question 6
Describe the formation of tissue fluid and its relationship with plasma. (5 marks)
Mark Scheme:
- Formation:
- Fluid leaks out of capillaries into the spaces between cells, forming tissue fluid. (1 mark)
- Composition Similarity:
- Contains water, ions, and small molecules similar to plasma. (1 mark)
- Exclusion of Large Proteins:
- Large proteins like albumin do not pass into tissue fluid, remaining in the blood. (1 mark)
- Exclusion of RBCs:
- Red blood cells do not pass into tissue fluid. (1 mark)
- Cell Movement:
- White blood cells (WBCs) can move through capillaries into tissue fluid to perform immune functions. (1 mark)
Question 7
Explain the concept of selective permeability in capillary walls and its relationship with molecular mass. (5 marks)
Mark Scheme:
- Selective Permeability:
- Small molecules (e.g., water, ions) pass through capillary walls easily. (1 mark)
- Large molecules (e.g., albumin) rarely pass through, remaining in the blood plasma. (1 mark)
- Relationship with Molecular Mass:
- Smaller Molecules: Higher permeability (e.g., Water with RMM 18, Permeability 1.00). (1 mark)
- Larger Molecules: Lower permeability (e.g., Albumin with RMM 69,000, Permeability 0.00001). (1 mark)
- Physiological Significance:
- Ensures that essential small molecules can reach cells while large proteins are retained in the blood to maintain osmotic balance. (1 mark)
Question 8
Define edema and explain its causes and prevention mechanisms. (5 marks)
Mark Scheme:
- Definition:
- Edema is the accumulation of excess fluid in tissues, leading to swelling. (1 mark)
- Causes:
- Excess Fluid Leakage: Can occur due to high blood pressure or damage to capillary walls. (1 mark)
- Prevention:
- Role of Arterioles: Regulate blood flow into capillaries, reducing pressure and minimizing fluid leakage. (1 mark)
- Additional Prevention:
- Lymphatic System: Drains excess tissue fluid to prevent fluid buildup. (1 mark)
- Clinical Significance:
- Preventing edema is crucial to maintain tissue integrity and prevent impaired function. (1 mark)
Question 9
Explain the role of arterioles in preventing edema. (4 marks)
Mark Scheme:
- Regulation of Blood Flow:
- Arterioles control the amount of blood entering the capillaries by vasoconstriction and vasodilation. (1 mark)
- Pressure Control:
- By reducing blood flow, arterioles help lower blood pressure within capillaries, minimizing fluid leakage into tissues. (1 mark)
- Preventing Excess Fluid Leakage:
- Vasoconstriction of arterioles decreases capillary hydrostatic pressure, reducing the force that drives fluid out of capillaries. (1 mark)
- Minimizing Edema Risk:
- Proper arteriole function ensures that fluid balance is maintained, preventing the accumulation of excess fluid in tissues (edema). (1 mark)
Question 10
Describe how homeostasis is maintained in the tissue fluid environment. (5 marks)
Mark Scheme:
- Definition of Homeostasis:
- Homeostasis is the maintenance of a stable internal environment within the body. (1 mark)
- Tissue Fluid Environment Stability:
- Must remain constant with optimal levels of glucose, pH, waste removal, and temperature for proper cell function. (1 mark)
- Regulatory Mechanisms:
- Blood-Brain Barrier: Protects the brain by regulating substance entry. (1 mark)
- Kidney Function: Regulates ion balance and waste removal through filtration and reabsorption. (1 mark)
- Hormonal Control: Maintains fluid balance and electrolyte levels via hormones like antidiuretic hormone (ADH) and aldosterone. (1 mark)
- Overall Maintenance:
- These mechanisms work together to ensure that internal conditions remain stable despite external changes, supporting cellular homeostasis. (1 mark)