8.08 Heart Anatomy and Blood Flow Dynamics
I. Anatomy of the Heart
- The heart is a muscular organ located in the thoracic cavity, central to the circulatory system. It comprises four chambers, valves, major blood vessels, and conduction systems that regulate its rhythmic contractions.
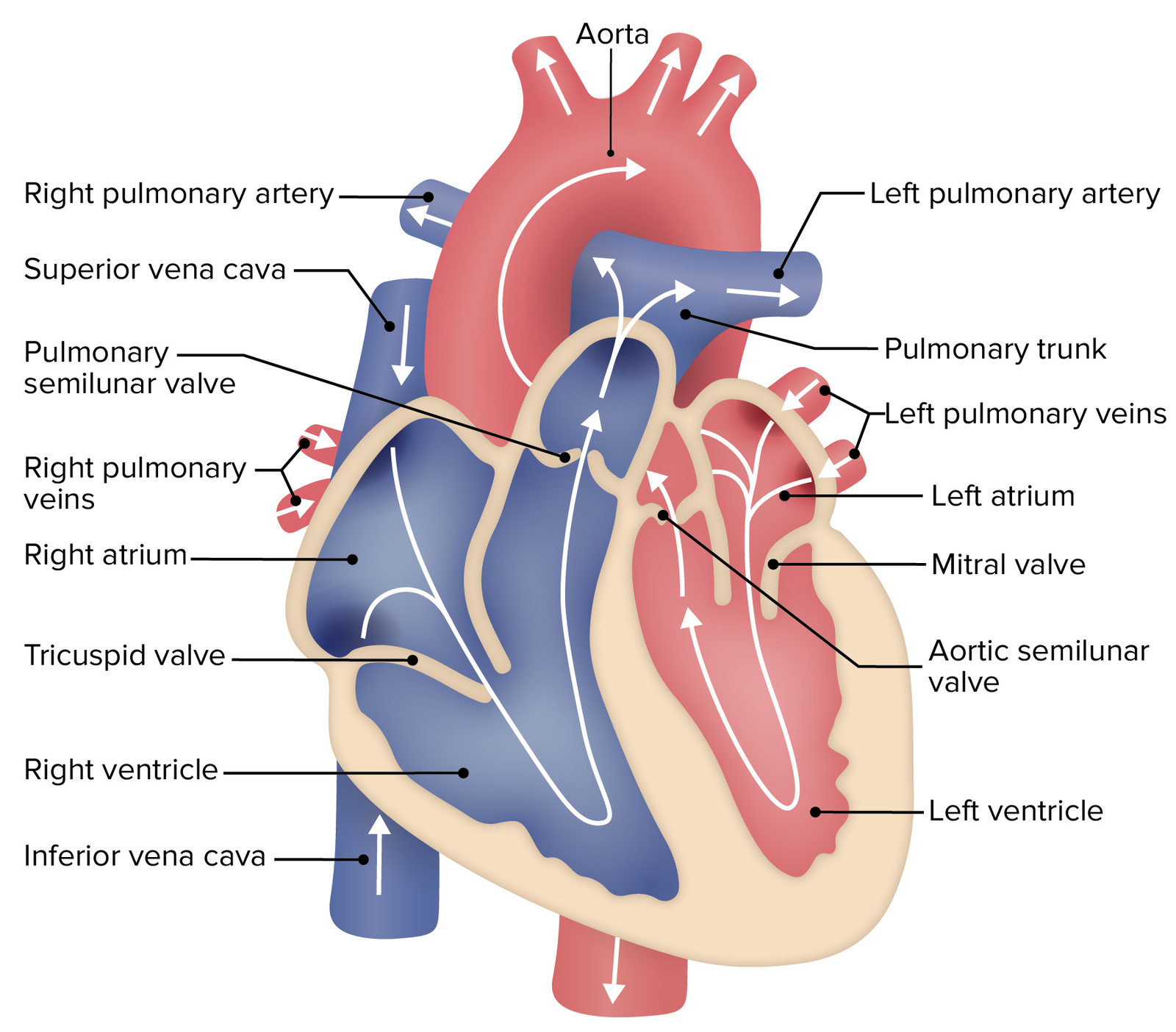
A. Chambers of the Heart
- Atria (Upper Chambers):
- Right Atrium (RA): Receives deoxygenated blood from the body via the superior and inferior vena cava.
- Left Atrium (LA): Receives oxygenated blood from the lungs via the pulmonary veins.
- Ventricles (Lower Chambers):
- Right Ventricle (RV): Pumps deoxygenated blood to the lungs through the pulmonary artery.
- Left Ventricle (LV): Pumps oxygenated blood to the body through the aorta. It has the thickest walls due to the high pressure required for systemic circulation.
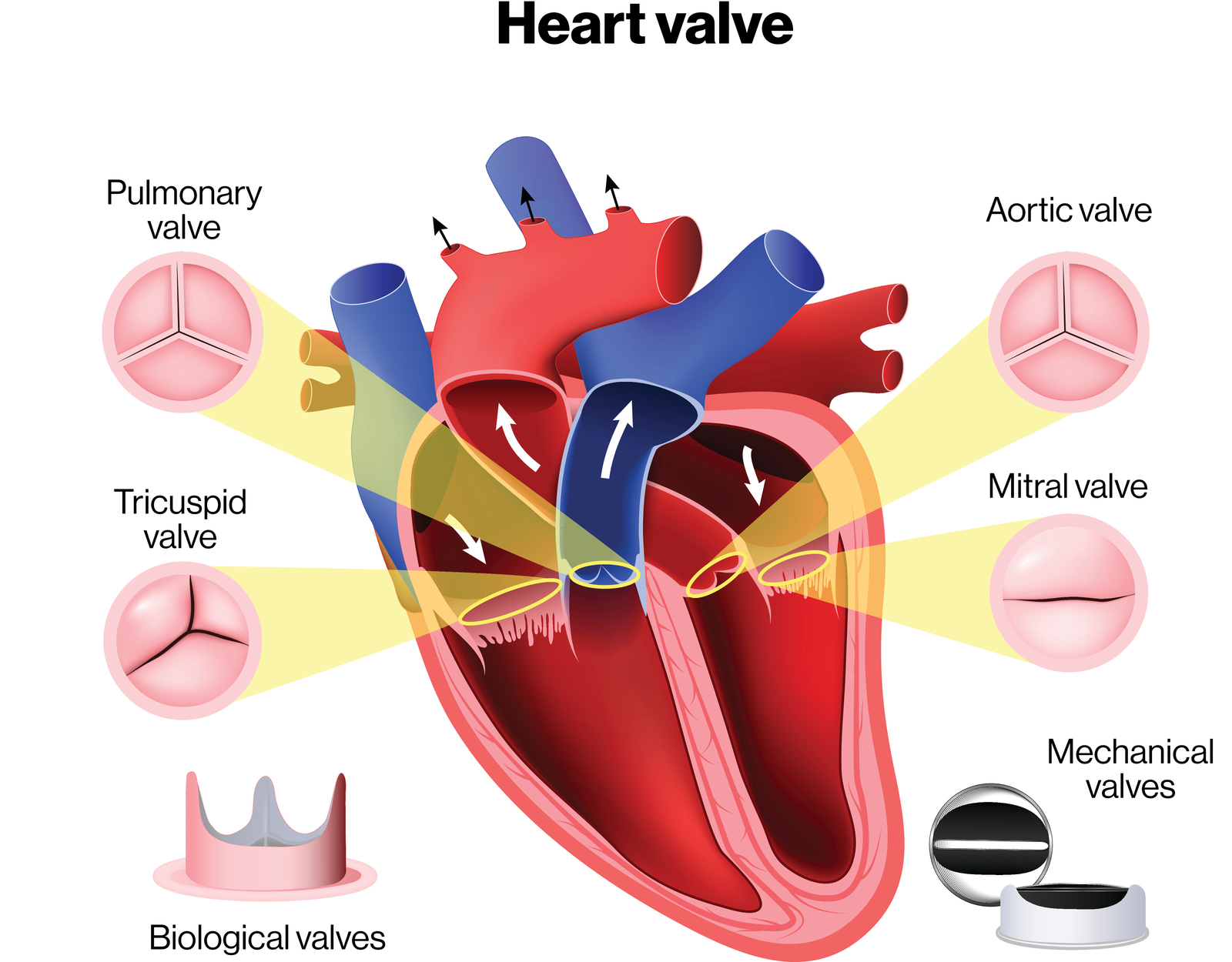
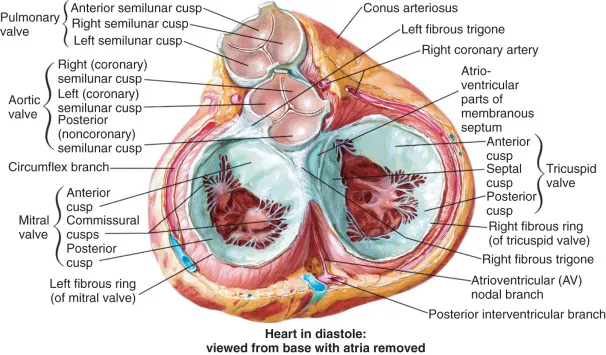
B. Heart Valves
- Valves ensure unidirectional blood flow and prevent backflow. There are four main valves:
- Atrioventricular (AV) Valves:
- Tricuspid Valve: Between RA and RV.
- Mitral (Bicuspid) Valve: Between LA and LV.
- Semilunar Valves:
- Pulmonary Valve: Between RV and pulmonary artery.
- Aortic Valve: Between LV and aorta.
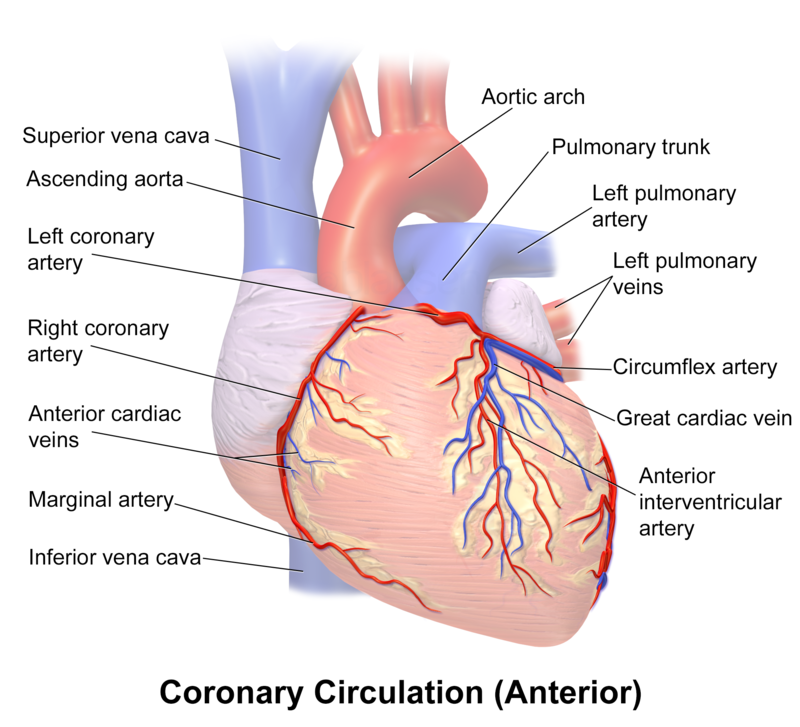
C. Major Blood Vessels
- Superior and Inferior Vena Cava: Bring deoxygenated blood to the RA.
- Pulmonary Arteries: Transport deoxygenated blood from RV to lungs.
- Pulmonary Veins: Carry oxygenated blood from lungs to LA.
- Aorta: Distributes oxygenated blood from LV to systemic circulation.
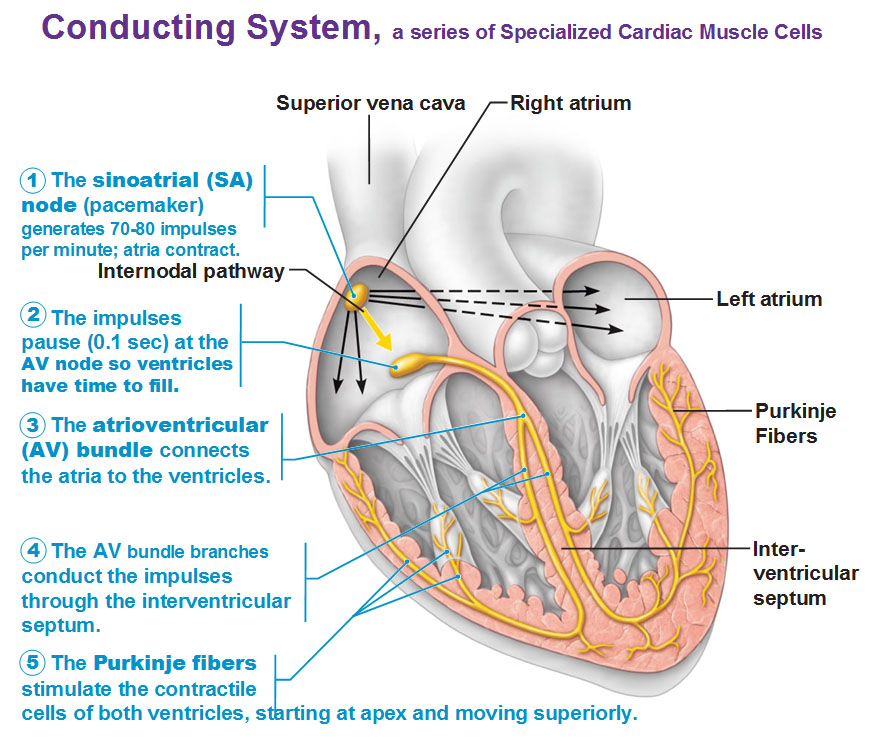
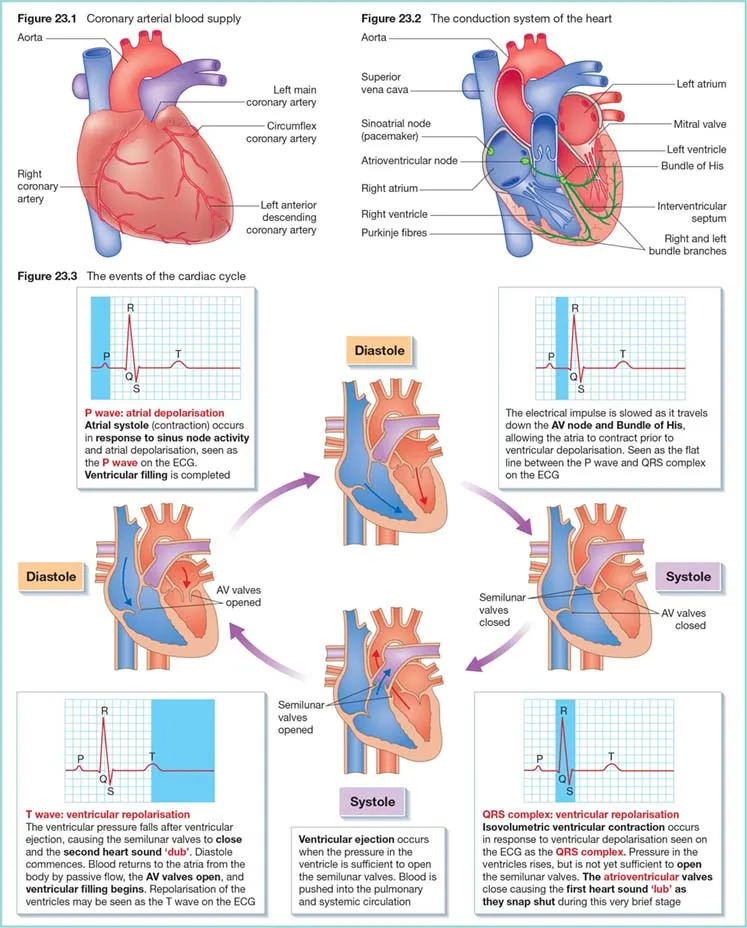
D. Conduction System
- Sinoatrial (SA) Node: Located in the RA; initiates electrical impulses (natural pacemaker).
- Atrioventricular (AV) Node: Located between atria and ventricles; delays impulses.
- Bundle of His and Purkinje Fibers: Conduct impulses to ventricular myocardium, triggering contraction.
II. Step-by-Step Blood Flow Through the Heart
- Understanding the sequential flow of blood through the heart is essential. Here’s a detailed, step-by-step process:
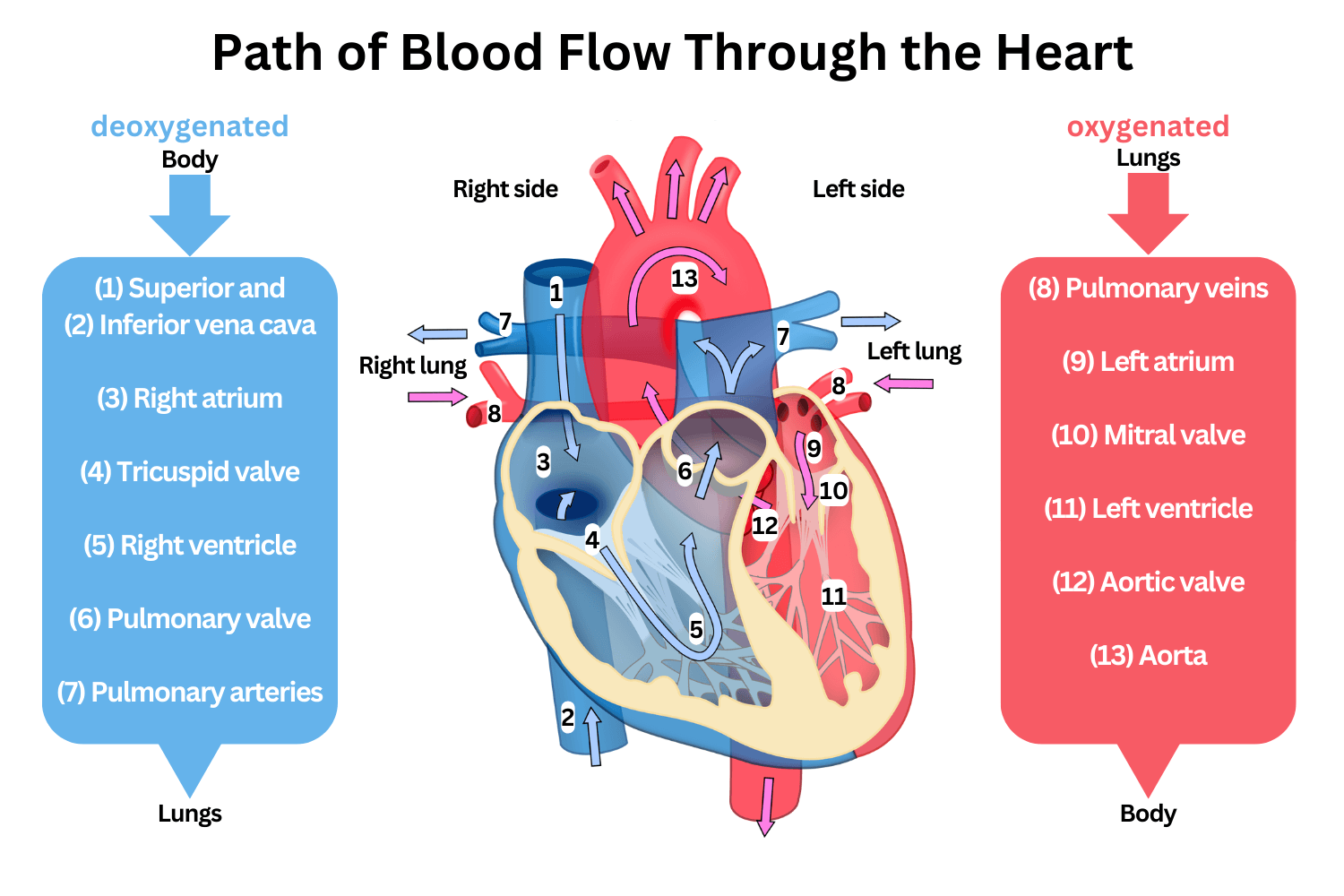
A. Blood Entry into the Heart
- Deoxygenated Blood Returns to the Heart:
- Via Superior and Inferior Vena Cava: Blood from the body enters the Right Atrium (RA).
- Passage Through the Tricuspid Valve:
- Tricuspid Valve Opens: During diastole (relaxation phase), the tricuspid valve opens, allowing blood to flow from RA to Right Ventricle (RV).
B. Blood Flow from Right Ventricle to Lungs
- Ventricular Contraction (Systole):
- Electrical Impulse: Initiated by the SA node, travels through the AV node and Bundle of His to Purkinje fibers, causing ventricular contraction.
- Tricuspid Valve Closes: Prevents backflow into RA.
- Pulmonary Valve Opens:
- Pulmonary Semilunar Valve: Opens, allowing blood to be ejected from RV into the Pulmonary Artery toward the lungs for oxygenation.
C. Oxygenated Blood Returns to the Heart
- Oxygenated Blood from Lungs:
- Pulmonary Veins: Four veins (two from each lung) carry oxygen-rich blood into the Left Atrium (LA).
- Passage Through the Mitral Valve:
- Mitral (Bicuspid) Valve Opens: During diastole, allows blood to flow from LA to Left Ventricle (LV).
D. Blood Flow from Left Ventricle to Body
- Left Ventricular Contraction (Systole):
- Electrical Impulse: Similar pathway as RV; causes LV contraction.
- Mitral Valve Closes: Prevents backflow into LA.
- Aortic Valve Opens:
- Aortic Semilunar Valve: Opens, allowing blood to be pumped from LV into the Aorta, distributing oxygenated blood to the systemic circulation.
E. Cycle Repeats
- Relaxation Phase (Diastole):
- Ventricles Relax: Semilunar valves close to prevent backflow from arteries.
- Atrioventricular Valves Open: To receive blood filling the atria again, and the cycle continues.

III. Heart Valves: Opening and Closing Mechanism
- Valves operate based on pressure gradients between heart chambers and major arteries.
A. Atrioventricular (AV) Valves
- Opening:
- During Diastole: When ventricular pressure falls below atrial pressure, AV valves open, allowing blood to flow from atria to ventricles.
- Closing:
- At the Onset of Systole: When ventricles begin to contract, ventricular pressure exceeds atrial pressure, causing AV valves to close, preventing backflow.
B. Semilunar Valves
- Opening:
- During Ventricular Systole: When ventricular pressure surpasses arterial pressure, semilunar valves open, allowing blood ejection into arteries.
- Closing:
- At the End of Systole (Early Diastole): When ventricular pressure falls below arterial pressure, semilunar valves close, preventing backflow into ventricles.
C. Importance of Valve Function
- Ensures Unidirectional Blood Flow: Prevents regurgitation and maintains efficient circulation.
- Prevents Mixing of Oxygenated and Deoxygenated Blood: Critical for maintaining oxygen delivery to tissues.
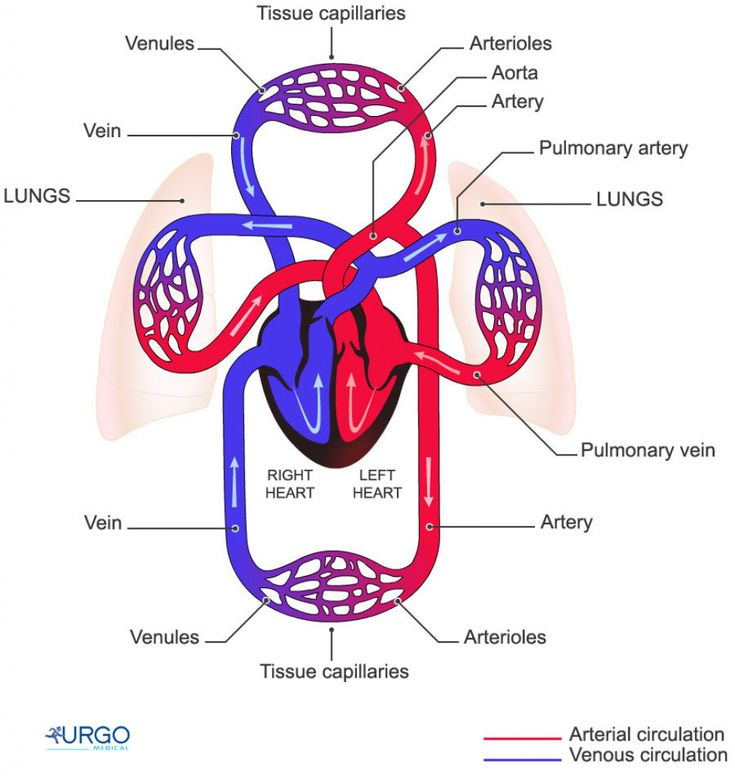
IV. Blood Flow Pathways: To the Aorta vs. To the Lungs
A. Systemic Circulation (To the Aorta and Body)
- Pathway:
- LV → Aortic Valve → Aorta → Arteries → Capillaries → Veins → Superior/Inferior Vena Cava → RA → RV → Pulmonary Artery → Lungs.
- Function:
- Delivers oxygenated blood to all body tissues.
- Returns deoxygenated blood to the heart.
B. Pulmonary Circulation (To the Lungs)
- Pathway:
- RV → Pulmonary Valve → Pulmonary Artery → Lungs → Pulmonary Veins → LA → LV → Aorta → Systemic Circulation.
- Function:
- Facilitates gas exchange (oxygenation of blood, removal of CO₂).
V. Pressure Dynamics in the Heart and Blood Vessels
- Understanding pressure changes is crucial for comprehending heart function and blood flow.
A. Cardiac Cycle Phases and Pressures
- Diastole (Relaxation Phase):
- Atria and Ventricles Relax: Ventricular pressure drops below atrial pressure.
- Pressure in Chambers:
- RA and LA have higher pressure than RV and LV, causing AV valves to open.
- Ventricular Filling: Blood flows passively from atria to ventricles.
- Systole (Contraction Phase):
- Ventricular Contraction:
- Isovolumetric Contraction: Ventricular pressure rises without blood ejection (all valves closed).
- Ventricular Pressure Exceeds Arterial Pressure: Semilunar valves open; blood is ejected.
- Ventricular Ejection:
- Aortic Pressure: LV pressure exceeds aortic pressure, blood flows into aorta.
- Pulmonary Pressure: RV pressure exceeds pulmonary artery pressure, blood flows into lungs.
- Ventricular Contraction:
- Pressure Values (Approximate):
1. Right Atrium (RA)
◉ Mean pressure: 0–8 mmHg
◉ During atrial contraction (a wave): ~6–8 mmHg
◉ During atrial relaxation (v wave): ~3–8 mmHg
◉ Lowest pressure (x descent): ~0–2 mmHg
🩸 Why so low? → The right atrium receives deoxygenated blood from the vena cavae, so it has low pressure to allow venous return.
2. Right Ventricle (RV)
◉ Diastolic (relaxed): 0–8 mmHg
◉ Systolic (contracting): 15–30 mmHg
🩸 Function: The right ventricle pumps blood into the pulmonary artery, but since it’s a low-resistance system, pressures are lower than in the left ventricle.
3. Pulmonary Artery (PA)
◉ Diastolic: 8–15 mmHg
◉ Systolic: 15–30 mmHg
◉ Mean PA pressure: ~10–20 mmHg
🩸 Why is this important? Pulmonary artery pressure must be low to avoid pulmonary edema and allow easy blood flow to the lungs.
4. Left Atrium (LA)
◉ Mean pressure: 4–12 mmHg
◉ During atrial contraction (a wave): ~10–12 mmHg
◉ During atrial relaxation (v wave): ~8–12 mmHg
🩸 Why higher than RA? → The left atrium receives oxygenated blood from the lungs, which have slightly higher pressure than systemic veins.
5. Left Ventricle (LV)
◉ Diastolic (relaxed): 3–12 mmHg
◉ Systolic (contracting): 90–140 mmHg
🩸 Why so high? → The left ventricle pumps blood into the aorta, which supplies the whole body, requiring high pressure to overcome systemic resistance.
6. Aorta
◉ Diastolic: 60–90 mmHg
◉ Systolic: 90–140 mmHg
◉ Mean Arterial Pressure (MAP): ~70–100 mmHg
🩸 Why so high? → The aorta distributes blood to all organs, so it must maintain constant pressure to ensure adequate perfusion.
B. Blood Pressure Regulation
- Systemic Arterial Pressure: Maintained by LV contraction force and arterial resistance.
- Venous Pressure: Lower than arterial pressure; veins act as blood reservoirs.
- Capillary Pressure: Balance between hydrostatic and osmotic pressures regulates fluid exchange.
VI. Step-by-Step Blood Flow and Pressure Changes
- To visualize the dynamic process, here’s a sequential breakdown:
1. Atrial Filling (Late Diastole)
- High Atrial Pressure: Blood flows into atria from veins.
- AV Valves Open: Blood moves into ventricles as ventricular pressure remains low.
2. Ventricular Filling (Early Systole)
- Ventricular Contraction Begins:
- Isovolumetric Contraction: Ventricles contract, increasing pressure without changing volume as AV valves close (preventing backflow).
- Pressure Build-Up: Ventricular pressure rises sharply.
3. Ventricular Ejection (Systole Continued)
- Semilunar Valves Open: Once ventricular pressure exceeds arterial pressure.
- Aortic Valve Opens: Blood is ejected into the aorta.
- Pulmonary Valve Opens: Blood is ejected into the pulmonary artery.
- Pressure Peak: Reaches systolic pressure (~120 mmHg in aorta).
4. Ventricular Relaxation (Diastole Initiation)
- Ventricular Ejection Ceases: Semilunar valves close as ventricular pressure falls below arterial pressure.
- Isovolumetric Relaxation: Ventricles relax without volume change; AV valves remain closed.
5. Ventricular Filling (Late Systole to Diastole)
- Pressure Drops: Ventricular pressure falls below atrial pressure.
- AV Valves Reopen: Blood flows from atria to ventricles, completing the cycle.
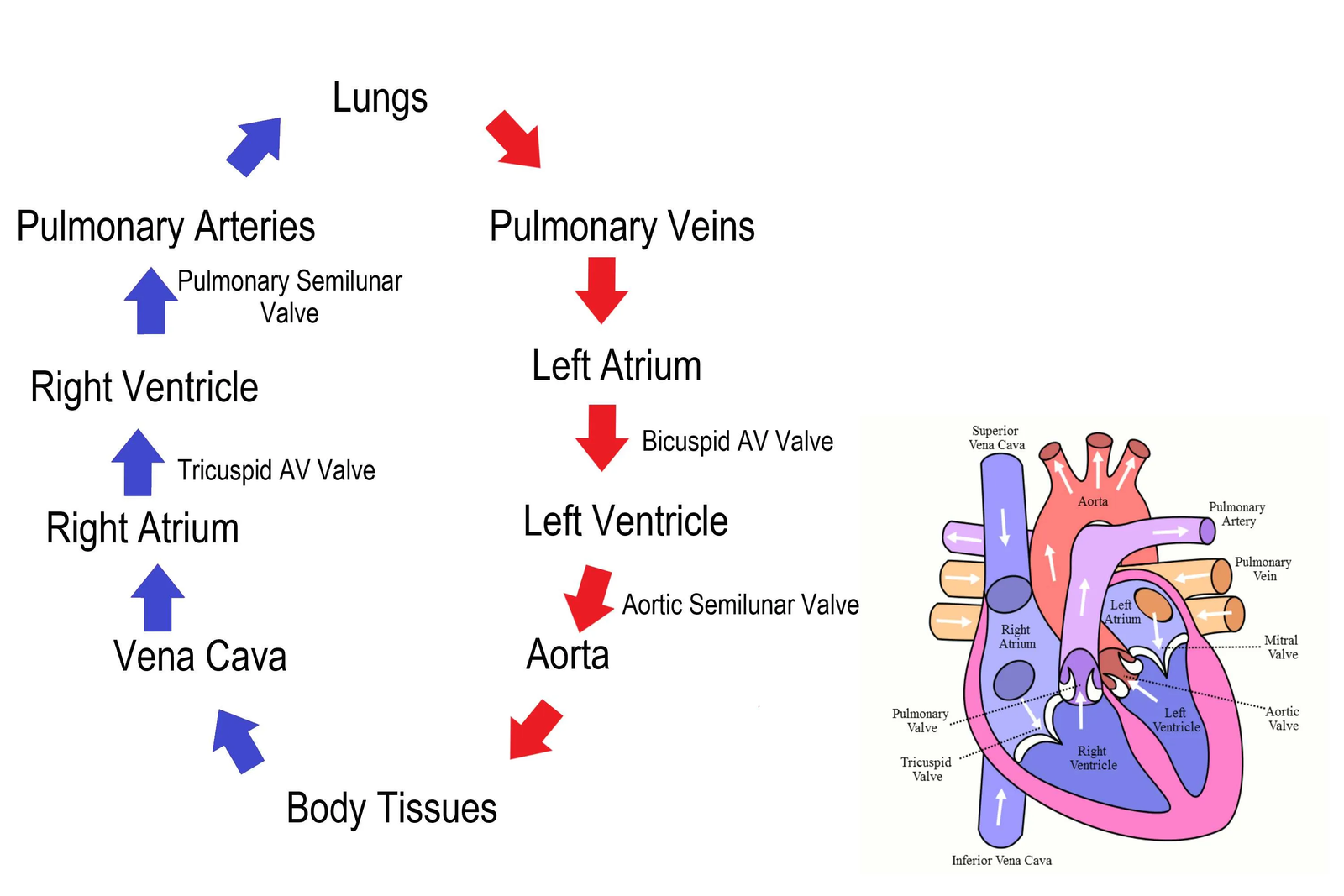
VII. Summary of Blood Flow Pathway
- Body → Superior/Inferior Vena Cava → Right Atrium (RA)
- RA → Tricuspid Valve → Right Ventricle (RV)
- RV → Pulmonary Valve → Pulmonary Artery → Lungs
- Lungs → Pulmonary Veins → Left Atrium (LA)
- LA → Mitral Valve → Left Ventricle (LV)
- LV → Aortic Valve → Aorta → Systemic Circulation → Body
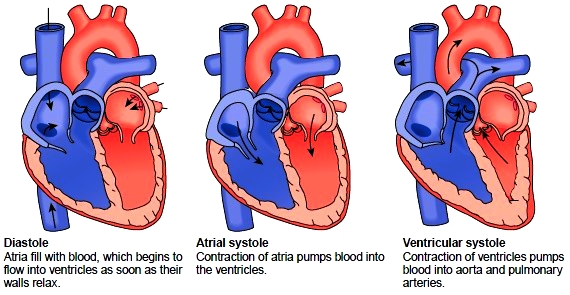
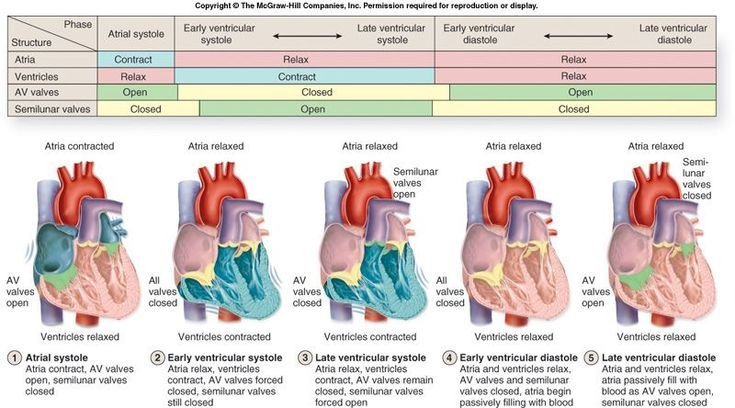
Cardiac Cycle: Detailed Breakdown of the Heartbeat Sequence
- The cardiac cycle consists of a series of events that occur during each heartbeat, encompassing periods of contraction (systole) and relaxation (diastole) of the heart chambers.
1. Atrial Systole – Contraction of Atria
- Action:
- Atria contract, pushing blood into the ventricles through the atrioventricular (AV) valves.
- Mechanism:
- Increased Atrial Pressure: Raises the pressure in the atria, causing the AV valves (bicuspid/mitral on the left and tricuspid on the right) to open.
- Valve Function:
- AV Valves Open: Allows blood flow from atria to ventricles.
- Semilunar Valves: Prevent backflow into the veins (vena cava and pulmonary veins) by remaining closed during atrial systole.
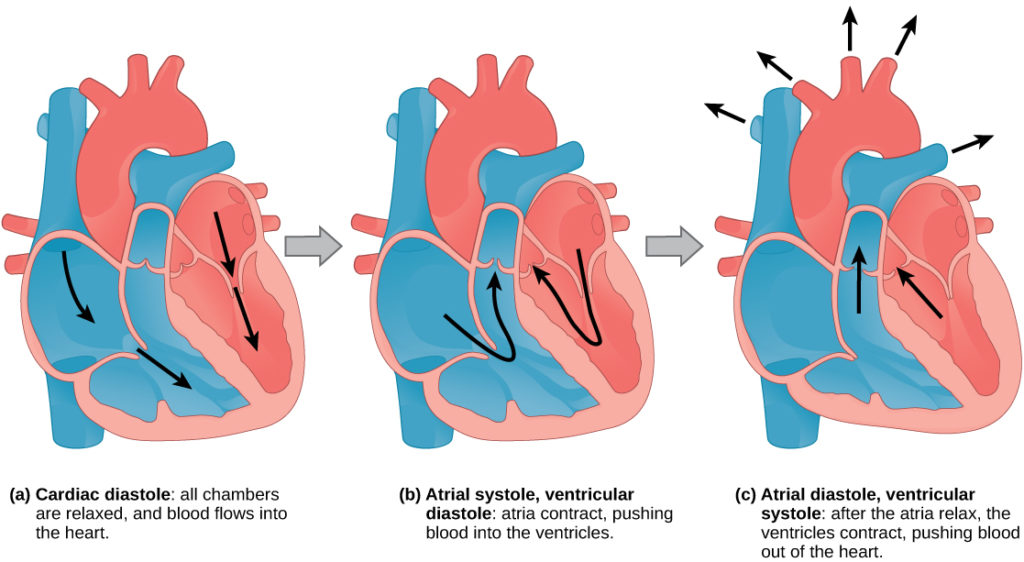
2. Ventricular Systole – Contraction of Ventricles
- Action:
- Ventricles contract, pushing blood into the arteries.
- Mechanism:
- High Ventricular Pressure: Closes the AV valves to prevent blood from flowing back into the atria.
- Semilunar Valves Open: Allows blood to flow from the left ventricle into the aorta and from the right ventricle into the pulmonary artery.
- Duration:
- Approximately 0.3 seconds.

3. Diastole – Relaxation of Heart Muscle
- Action:
- Both atria and ventricles relax, allowing the heart chambers to refill with blood.
- Mechanism:
- Low Ventricular Pressure:
- AV Valves Open: Allows blood to flow from the veins (vena cava and pulmonary veins) into the relaxed atria and trickle into the ventricles.
- Semilunar Valves Close:
- Prevention of Backflow: Snaps shut to prevent arterial blood from flowing back into the ventricles as ventricular pressure drops.
- Low Ventricular Pressure:
Heart Valve Function in the Cardiac Cycle
- Heart valves ensure unidirectional blood flow through the heart’s chambers and prevent backflow during different phases of the cardiac cycle.
Atrioventricular (AV) Valves
- Types:
- Bicuspid (Mitral) Valve: Located between the left atrium and left ventricle.
- Tricuspid Valve: Located between the right atrium and right ventricle.
- Function During Cardiac Cycle:
- Atrial Systole:
- Open: Allows blood to flow from atria to ventricles.
- Ventricular Systole:
- Closed: Prevents blood from flowing back into atria.
- Atrial Systole:
- Supporting Structures:
- Papillary Muscles and Tendons:
- Role: Stabilize the AV valves by preventing them from inverting under high ventricular pressure.
- Papillary Muscles and Tendons:
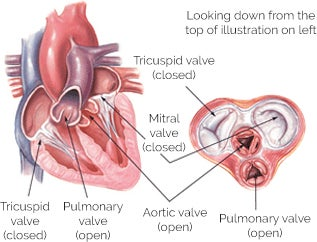
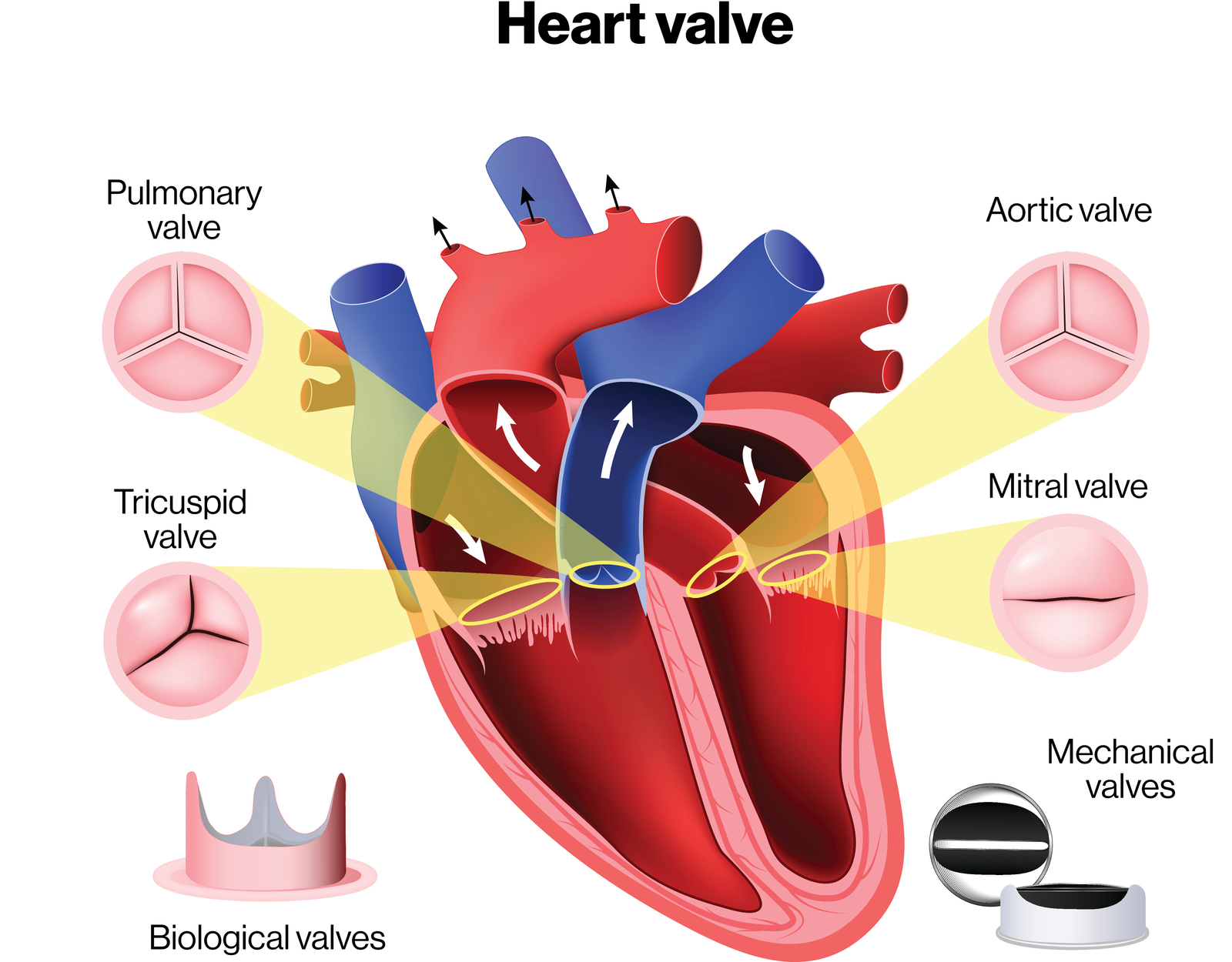
Semilunar Valves
- Types:
- Aortic Valve: Located between the left ventricle and the aorta.
- Pulmonary Valve: Located between the right ventricle and the pulmonary artery.
- Function During Cardiac Cycle:
- Ventricular Systole:
- Open: Allows blood to flow from ventricles into arteries.
- Diastole:
- Closed: Prevents blood from flowing back into ventricles from the arteries.
- Ventricular Systole:
Pressure Dynamics and Structural Adaptations in Heart Chambers
- The heart’s structure is adapted to handle different pressure requirements in various chambers, ensuring efficient blood flow to both the lungs and the rest of the body.
Ventricles vs. Atria
- Ventricular Walls:
- Thicker Muscular Walls:
- Reason: Generate higher pressures required to pump blood throughout the body (left ventricle) and into the lungs (right ventricle).
- Thicker Muscular Walls:
- Atrial Walls:
- Thinner Walls:
- Reason: Atria only need to pump blood into ventricles, requiring less force.
- Thinner Walls:
Left Ventricle
- Structural Features:
- Thick Muscular Wall: Necessary for generating high pressure.
- Function:
- Systemic Circulation: Pumps oxygenated blood into the aorta to supply the entire body.
- Pressure Maintenance: Ensures sufficient pressure for blood to reach distant organs, even during high-demand situations like exercise.
Right Ventricle
- Structural Features:
- Thinner Muscular Wall: Adequate for lower pressure requirements.
- Function:
- Pulmonary Circulation: Pumps deoxygenated blood into the pulmonary artery to supply the lungs.
- Pressure Regulation: Prevents excessive pressure in lung capillaries, protecting delicate lung tissues from damage.
Heart Sounds: Lub-Dub

Lub (S1):
- Happens when the heart’s valves between the upper and lower chambers (mitral and tricuspid valves) close.
- Signals the start of the heartbeat (when the heart pumps blood out).
- Best heard at the bottom of the heart.
Dub (S2):
- Happens when the valves to the big arteries (aortic and pulmonary valves) close.
- Signals the end of the heartbeat (when the heart relaxes to fill with blood).
- Best heard at the top of the heart.
Extra Notes:
- The heart sound is like a “lub-dub” rhythm.
- Doctors use a stethoscope to listen for these sounds and check if the heart is healthy.
- Any extra sounds might mean the heart valves aren’t working perfectly.