10.03 Malaria

1. Overview & Causative Agents
- Definition:
Malaria is a life-threatening parasitic disease primarily affecting tropical and subtropical regions.
- Causative Agents (Pathogens):
Four species of the protozoan genus Plasmodium are responsible for malaria in humans:- Plasmodium falciparum: Most severe and deadly.
- P. vivax
- P. ovale
- P. malariae
- Disease Vector:
Female Anopheles mosquitoes (approximately 30 species) are the primary vectors transmitting malaria. - Transmission Modes:
- Primary: Bites from infected female Anopheles mosquitoes.
- Secondary:
- Blood transfusions
- Sharing unsterile needles
- Mother-to-fetus (congenital transmission)
2. Transmission of Malaria
2.1 Mosquito-Borne Transmission
- Mechanism:
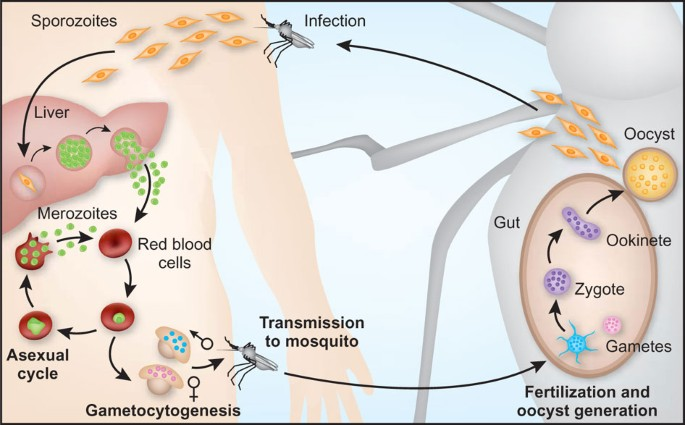
- Ingestion: An Anopheles mosquito bites an infected individual, ingesting gametocytes (sexual forms) of Plasmodium.
- Fertilization: Gametes fuse in the mosquito’s gut to form zygotes.
- Sporozoite Formation: Zygotes develop into motile sporozoites.
- Migration: Sporozoites migrate to the mosquito’s salivary glands.
- Infection: Upon the next bite, sporozoites are injected into a new host, initiating infection.
- Incubation Period:
Symptoms typically manifest 7–30 days post-infection, varying by Plasmodium species. P. falciparum often results in the most severe clinical presentations.
2.2 Human Infection Process
- Site of Action:
- Liver Stage: Sporozoites infect hepatocytes, multiplying asexually.
- Erythrocytic Stage: Merozoites invade red blood cells (RBCs), undergoing further asexual replication.
- Pathophysiology:
- RBC Rupture: Infected RBCs burst, releasing merozoites and causing symptoms.
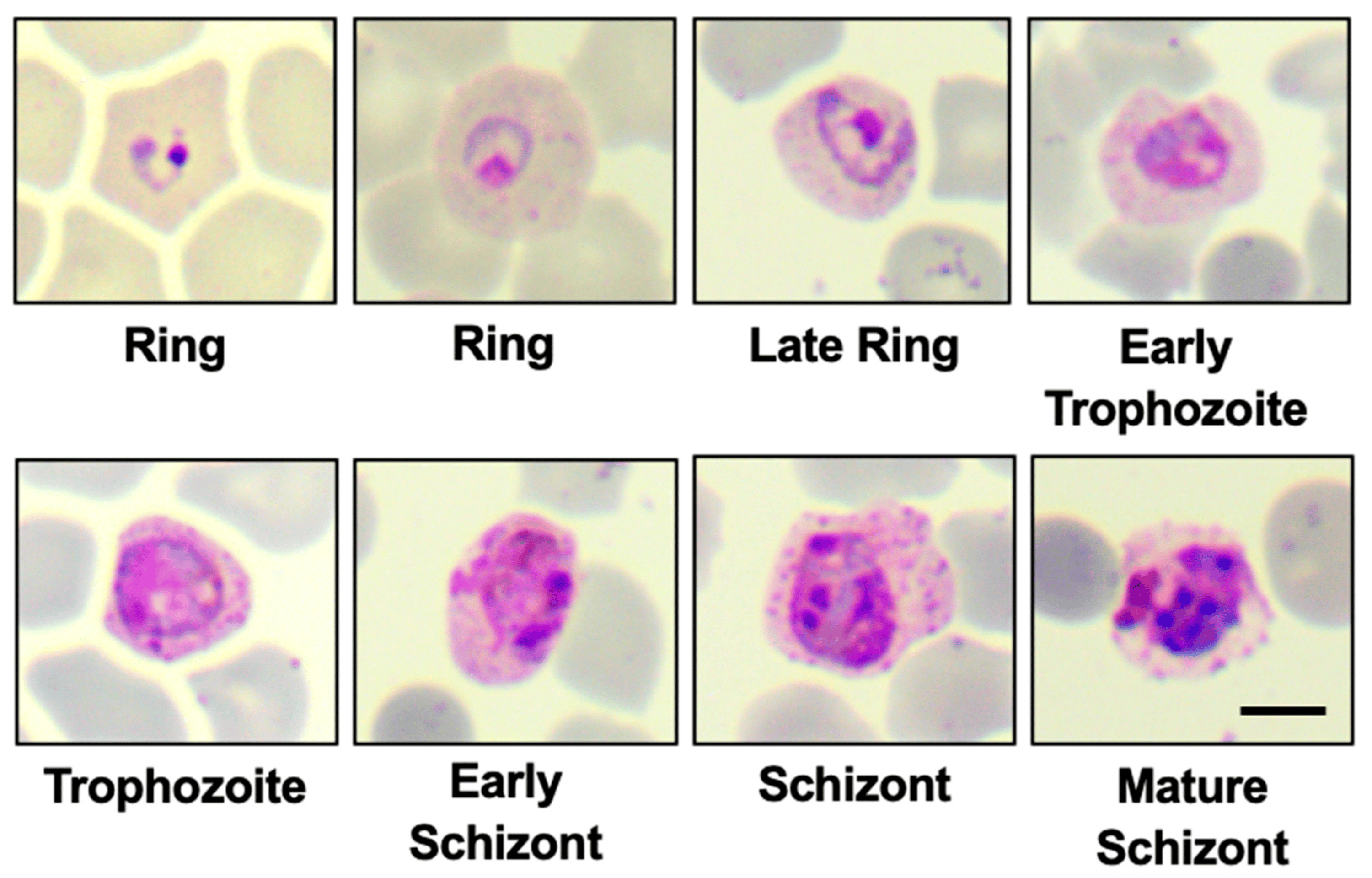
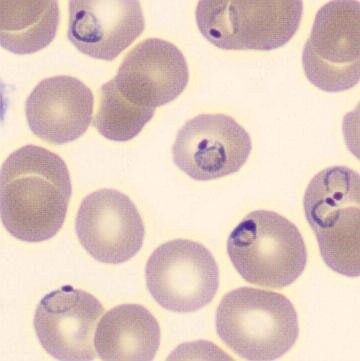
- Ring Forms: Plasmodium within RBCs appear as “signet ring” structures under microscopy.
- Parasite Proliferation: Each rupture releases multiple merozoites, escalating infection and transmission potential.
3. Transmission
From Infected RBCs to a New Mosquito
- 1. Asexual Replication in Humans:
- Invasion:
Plasmodium sporozoites (introduced by a mosquito bite) initially infect liver cells, then invade red blood cells (RBCs). - Asexual Multiplication:
Inside RBCs, the parasites multiply asexually, forming merozoites that continue the infection.
- Invasion:
- 2. Differentiation into Gametocytes (Gametocytogenesis):
- Development:
A subset of the parasites in RBCs differentiates into sexual forms called gametocytes (male and female) rather than continuing asexual replication. - Circulation:
These gametocytes remain in the bloodstream, waiting to be ingested by a mosquito.
- Development:
- 3. Mosquito Ingestion:
- Blood Meal:
When a female Anopheles mosquito bites an infected person, it ingests blood containing gametocytes.
- Blood Meal:
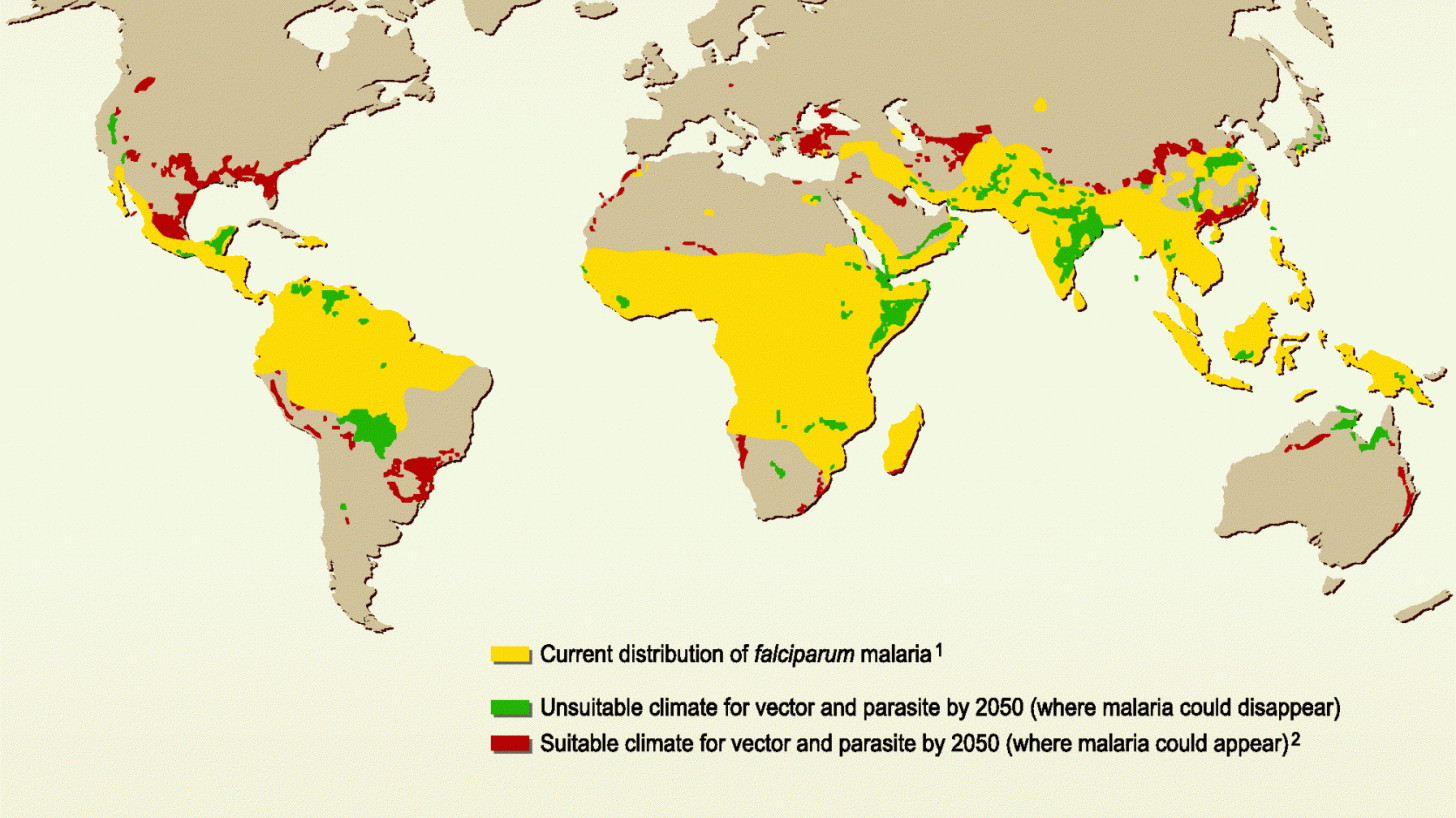
4. Environmental Factors
- Climatic Influence:
- Favorable Conditions: Warm, humid, and rainy climates enhance mosquito breeding and survival rates.
- Endemic Regions:
- Sub-Saharan Africa: Highest malaria burden due to efficient, long-lived Anopheles species.
- Seasonal Transmission:
- Rainy Seasons: Increase mosquito populations, leading to malaria epidemics, especially among non-immune individuals.

5. Clinical Features
| Feature | Details |
|---|---|
| Pathogen | P. falciparum, P. vivax, P. ovale, P. malariae |
| Transmission | Female Anopheles mosquito; other modes include blood transfusion, needle sharing, congenital. |
| Global Distribution | Predominantly in tropical and subtropical regions; endemic in 106 countries. |
| Incubation Period | 1 week to 1 year, depending on Plasmodium species. |
| Site of Action | Liver, red blood cells, brain (in severe cases, especially P. falciparum). |
| Clinical Features | Fever, anemia, nausea, headaches, muscle pain, shivering, sweating, enlarged spleen. |
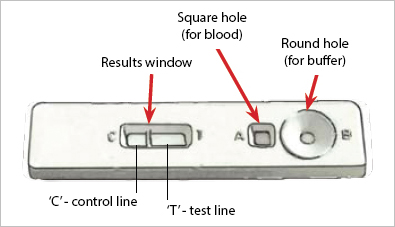
| Diagnosis | Antigen-based dipstick tests, microscopic examination of blood smears. |
| 2017 Statistics | 219 million cases globally; 92% in Africa. 435,000 deaths; 93% in Africa. |
6. Treatment of Malaria
6.1 Diagnosis
- WHO Recommendations:
Confirm suspected malaria cases using diagnostic tests detecting Plasmodium antigens. - Diagnostic Methods:
- Rapid Diagnostic Tests (RDTs): Provide results within 30 minutes.
- Microscopy: Gold standard; involves blood smear examination for parasite identification.
6.2 Treatment Options
- Antimalarial Drugs:
- Quinine: Inhibits parasite’s DNA and RNA synthesis.
- Chloroquine: Blocks heme polymerization in the parasite; widespread resistance observed.
- Proguanil: Inhibits dihydrofolate reductase, preventing parasite replication; also acts prophylactically.
- Drug Resistance:
- Challenges: High in regions with extensive drug usage (e.g., South America, Africa, Southeast Asia).
- Alternatives:
- Mefloquine: Effective but associated with neuropsychiatric side effects.
- Artemisinin-Based Combination Therapies (ACTs): Combine artemisinin derivatives with partner drugs for enhanced efficacy, particularly against P. falciparum.

Antimalarial medications have been instrumental in reducing malaria-related morbidity and mortality. However, their effectiveness has been compromised due to the malaria parasite’s ability to develop resistance. This resistance arises through genetic mutations that enable the parasite to survive despite drug treatment.
Factors Contributing to Antimalarial Drug Resistance:
- Genetic Mutations in Parasites:
- Plasmodium falciparum, the most lethal malaria parasite, has developed resistance to nearly all antimalarial drugs, including chloroquine, sulfadoxine/pyrimethamine, mefloquine, and quinine.
- Mutations in specific genes, such as the kelch13 gene, have been linked to artemisinin resistance. These genetic changes alter the parasite’s biology, reducing drug efficacy.
- Incomplete or Inconsistent Treatment:
- Patients not completing the full course of antimalarial therapy can leave surviving parasites, which may develop resistance.
- Self-medication and unregulated drug use contribute to subtherapeutic dosing, fostering resistance.
- Monotherapy Usage:
- Using a single antimalarial drug (monotherapy) increases the likelihood of resistance development. Combination therapies are preferred to reduce this risk.
- Counterfeit and Substandard Medications:
- The circulation of fake or low-quality antimalarial drugs leads to inadequate treatment, promoting resistance.
Current Challenges:
- Artemisinin Resistance: First identified in Southeast Asia, artemisinin resistance has now been observed in Africa. A 2024 study in Uganda reported that approximately 11% of children with severe malaria exhibited partial resistance to artemisinin.
- Spread of Resistance: The mobility of human populations and mosquitoes facilitates the spread of resistant parasite strains across regions, complicating malaria control efforts.
Strategies to Combat Resistance:
- Combination Therapies: Utilizing artemisinin-based combination therapies (ACTs) pairs artemisinin with a partner drug, enhancing treatment efficacy and reducing the potential for resistance development.
- Surveillance and Monitoring: Continuous monitoring of antimalarial drug efficacy helps in early detection of resistance patterns, enabling timely policy adjustments.
- Research and Development: Investing in the development of new antimalarial compounds and vaccines is crucial to stay ahead of emerging resistant strains.
6.3 Prophylactic (Preventive) Treatment
- The term prophylactic generally refers to something intended to prevent disease or a specific condition.
- Usage:
Recommended for travelers to endemic areas and high-risk groups (e.g., pregnant women, young children). - Mechanism:
Prevents parasite development following mosquito transmission. - Considerations:
- Avoiding Misdiagnosis: Particularly important in non-endemic regions where malaria may be confused with other febrile illnesses like influenza.
7. Prevention of Malaria
7.1 Vector Control Strategies
- Reduce Mosquito Population:
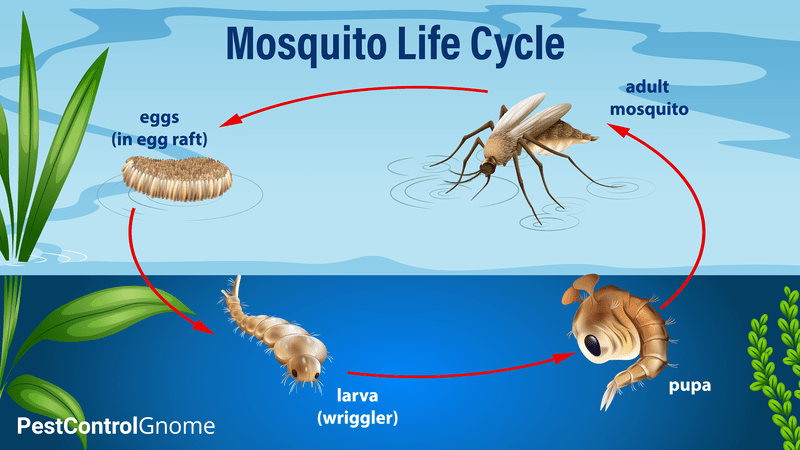
- Water Management: Eliminate or manage standing water to disrupt mosquito breeding.
- Larvicides: Apply oils (a thin layer of oil on the water suffocates larva) or biological agents like the bacteria Bacillus thuringiensis kills larvae.
- Biological Controls:
- Fish Introduction: Introduce larvivorous fish to water bodies to consume mosquito larvae.
- Avoid Mosquito Bites:
- Protective Clothing: Wear long sleeves and pants, especially during peak mosquito activity (dusk).
- Insect Repellents: Apply to skin and clothing.
- Insecticide-Treated Nets (ITNs): Utilize bed nets treated with insecticides to repel and kill mosquitoes, significantly reducing mortality.
- Indoor Residual Spraying (IRS): Apply insecticides to indoor surfaces; efficacy lasts up to six months depending on the product and environment.


7.2 Prophylactic Measures
- Drug Administration:
High-risk groups receive prophylactic antimalarials during periods of high transmission. - WHO Recommendations:
- Pregnant Women: Receive prophylactic drugs during antenatal care visits.
- Infants: In high-transmission areas, receive prophylactic doses during routine vaccinations.
8. Recent Advances in Malaria Control
- Diagnostics:
Enhanced rapid diagnostic tests (RDTs) enable prompt, on-site detection of malaria. - Genomic Research:
Complete sequencing of the Plasmodium genome facilitates the development of new drugs and vaccines. - Vaccination:
- RTS,S/AS01 (Mosquirix): The first malaria vaccine providing partial immunity, primarily in children.
- Pilot Programs: Initiated in Ghana, Kenya, and Malawi in 2019; ongoing development of additional vaccines.
- Global Support:
International funding and initiatives aim to reduce malaria prevalence in impoverished regions, supported by global foundations and philanthropic efforts.

9. Data Analysis Example: Zanzibar (1999-2008)


9.1 Data Description
- Trend: graph depictes the fluctuating but overall declining malaria cases and deaths in Zanzibar hospitals from 1999 to 2008.
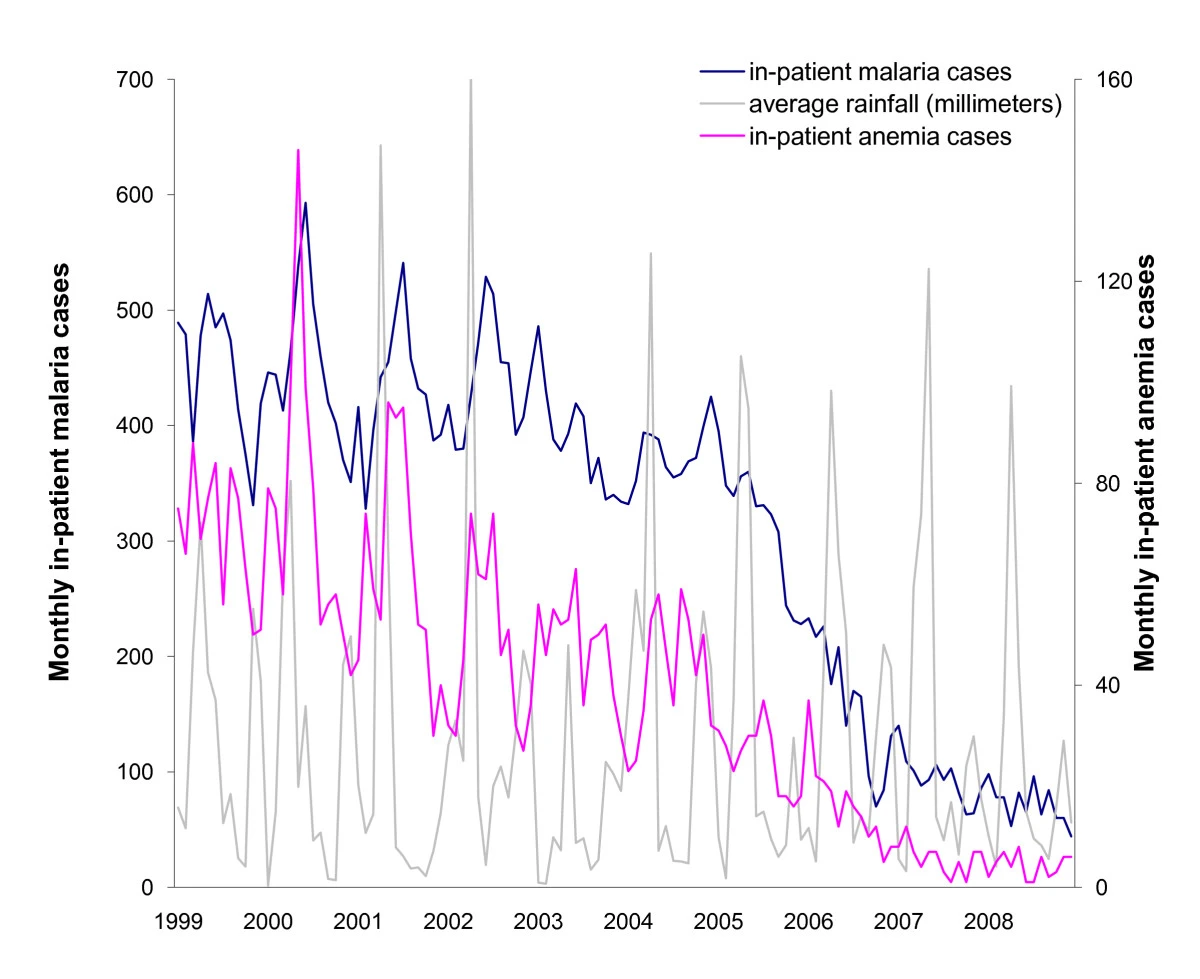

9.2 Possible Reasons for the Pattern
- Improved Control Measures:
Implementation of ITNs, increased access to effective antimalarial drugs, and enhanced public health initiatives.
9.3 Additional Data for Comprehensive Analysis
- ITN Usage Rates:
Percentage of households utilizing insecticide-treated nets. - Mosquito Population Density:
Data on Anopheles mosquito prevalence and breeding sites. - Local Climate Conditions:
Information on rainfall patterns, temperature, and humidity affecting mosquito lifecycle.
10. Challenges in Malaria Control
- Environmental Dependency:
Reliance on specific climatic conditions limits control measures to certain regions. - Mosquito Adaptation:
Anopheles mosquitoes exhibit adaptability and longevity, sustaining transmission cycles. - Seasonal Fluctuations:
Variations in mosquito populations due to seasonal changes complicate control efforts. - Drug Resistance:
Emergence of Plasmodium strains resistant to common antimalarials hampers treatment efficacy. - Socioeconomic Barriers:
Poverty and limited access to healthcare services impede effective malaria prevention and treatment.
11. Precautions for Avoiding Malaria
- Use of ITNs and Insect Repellents:
Employ bed nets and apply repellents to minimize mosquito bites. - Protective Clothing:
Wear long-sleeved garments and pants, especially during mosquito-active periods. - Prophylactic Antimalarial Drugs:
Administrate preventive medications to individuals traveling to or residing in endemic areas.
Questions
Describe How Malaria is Transmitted
- Answer: Malaria is primarily transmitted through the bite of an infected female Anopheles mosquito, which injects Plasmodium parasites into the human bloodstream along with its saliva. Additionally, transmission can occur via blood transfusions, sharing unsterile needles, and from mother to fetus during pregnancy.
How Do Plasmodium Cells Differ from Red Blood Cells?
- Answer: Plasmodium cells are eukaryotic protozoans containing organelles such as a nucleus, mitochondria, and other cellular structures. In contrast, human red blood cells (RBCs) are non-nucleated and lack organelles, optimized solely for oxygen transport.