9.05 Alveoli and Gas Exchange
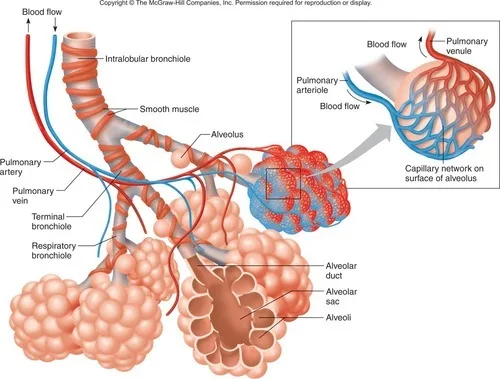
1. Structure and Function of Alveoli
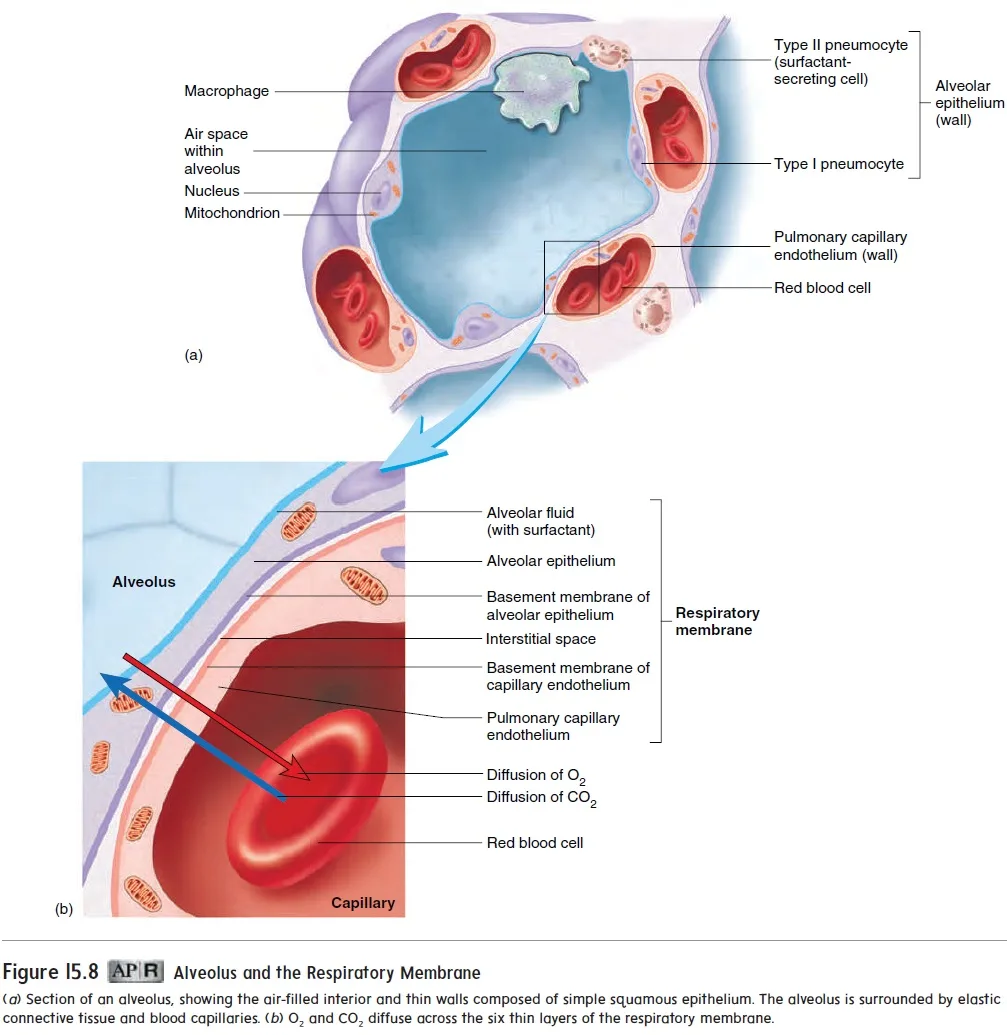
Location
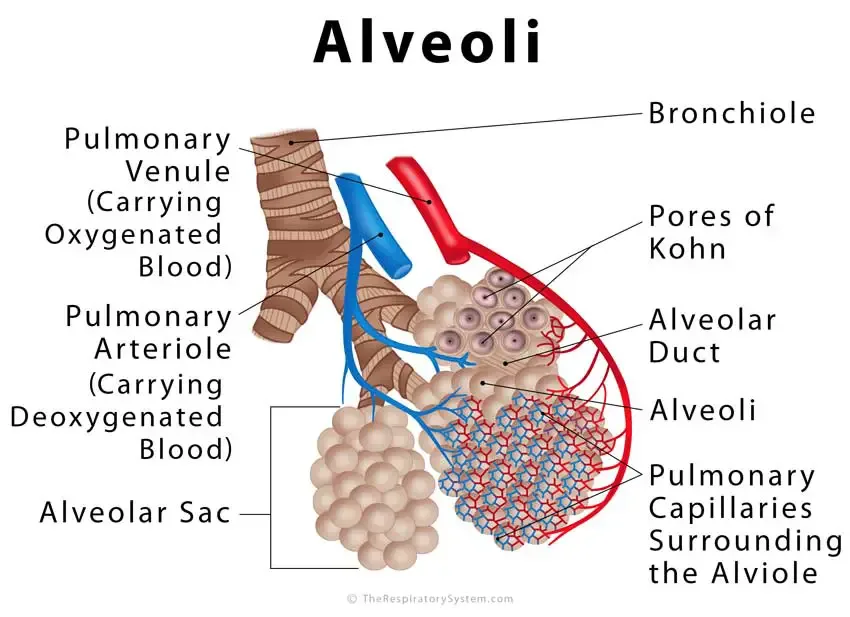
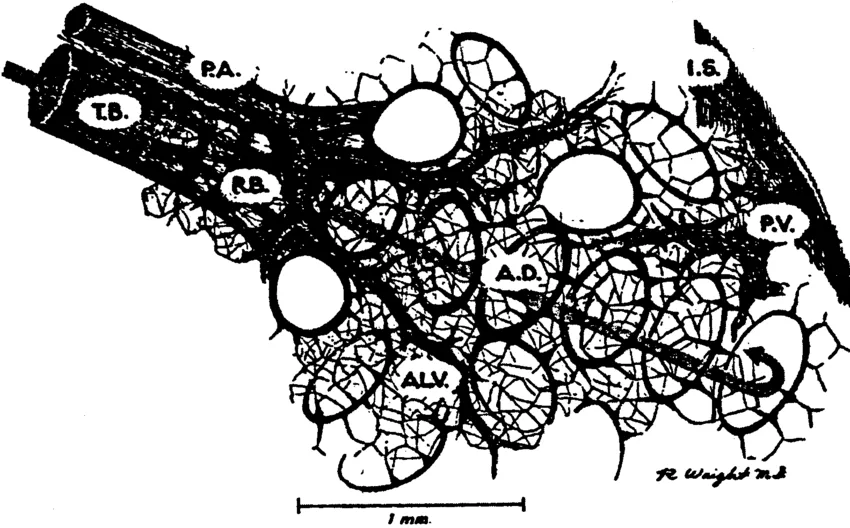
- Position in Respiratory Pathway:
- Alveoli are located at the terminal ends of the respiratory pathway, connected via bronchioles and alveolar ducts within the lungs.
Function
- Primary Site for Gas Exchange:
- Alveoli facilitate the exchange of oxygen (O₂) and carbon dioxide (CO₂) between inhaled air and the bloodstream.
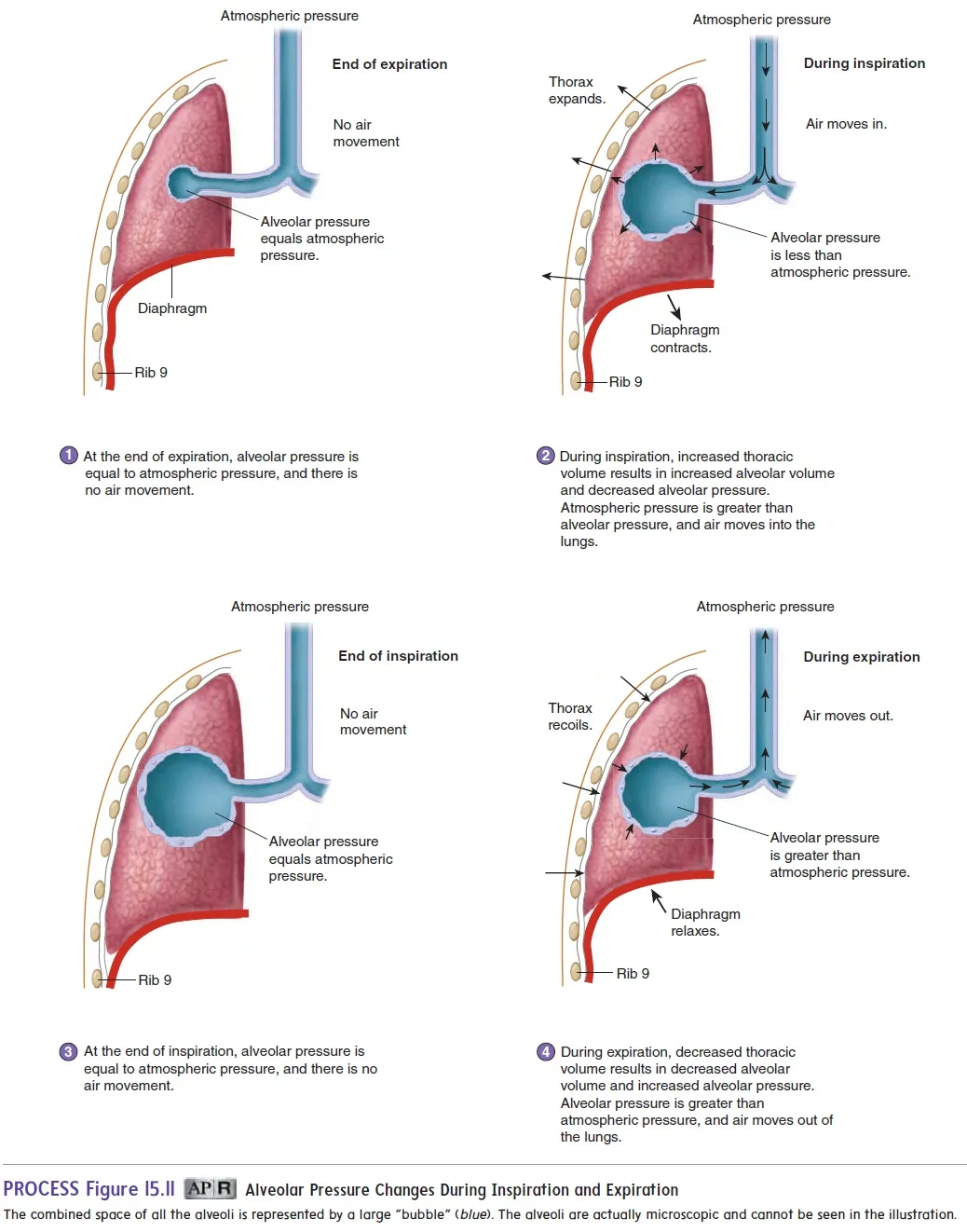
Elastic and Collagen Fibers
Elastic Fibers
- Role in Mechanics:
- Stretching: Allow alveoli to expand during inhalation.
- Recoil: Enable alveoli to return to their original shape during exhalation.
- Functional Benefits:
- Enhanced Diffusion: Expansion increases surface area during activities like exercise, promoting efficient gas exchange.
- Air Expulsion: Facilitates the effective expulsion of air from the lungs.
Collagen Fibers
- Structural Support:
- Prevention of Overstretching: Maintain alveolar integrity by preventing excessive stretching and potential rupture.
- Functional Benefits:
- Stability: Provide the necessary framework to keep alveoli open and structurally sound.
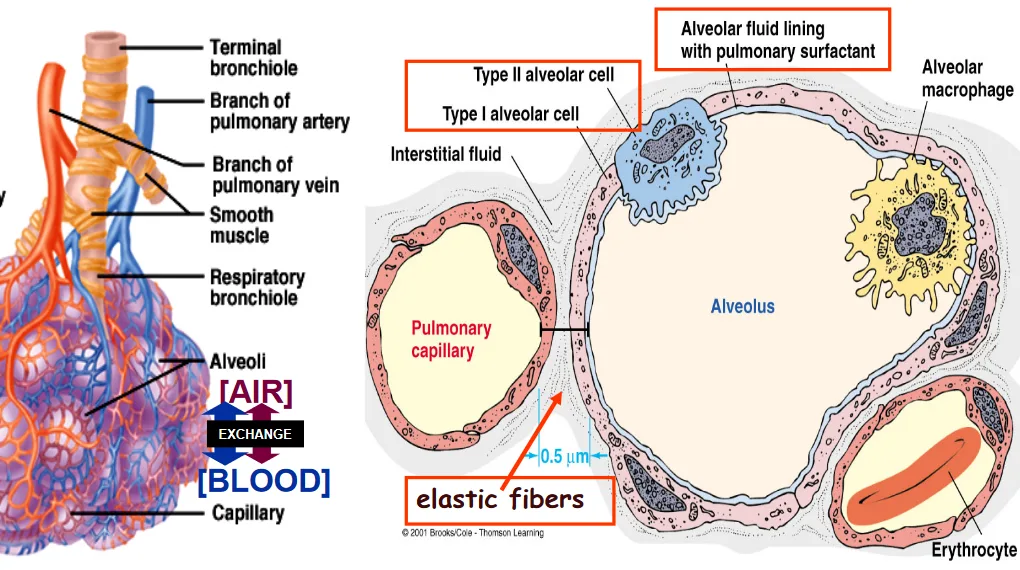
2. Structural Adaptations of Alveolar Walls
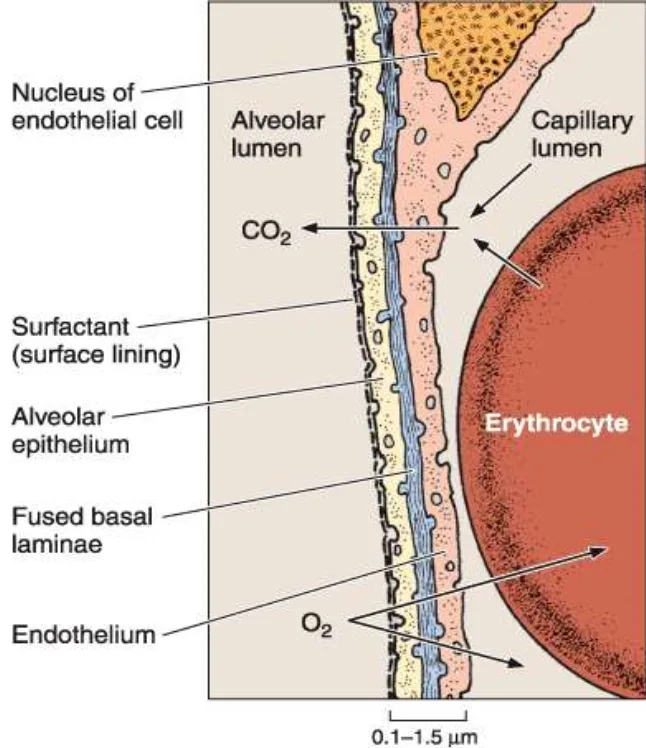
Thin Wall Structure
- Cellular Composition:
- Single Layer: Comprised of a single layer of squamous epithelial cells (Type I alveolar cells).
- Minimal Thickness: Cells are approximately 0.5 μm thick with cytoplasm layers as thin as 25 nm.
- Functional Advantage:
- Efficient Diffusion: Minimizes the distance for gas molecules to travel, facilitating rapid and efficient gas exchange.
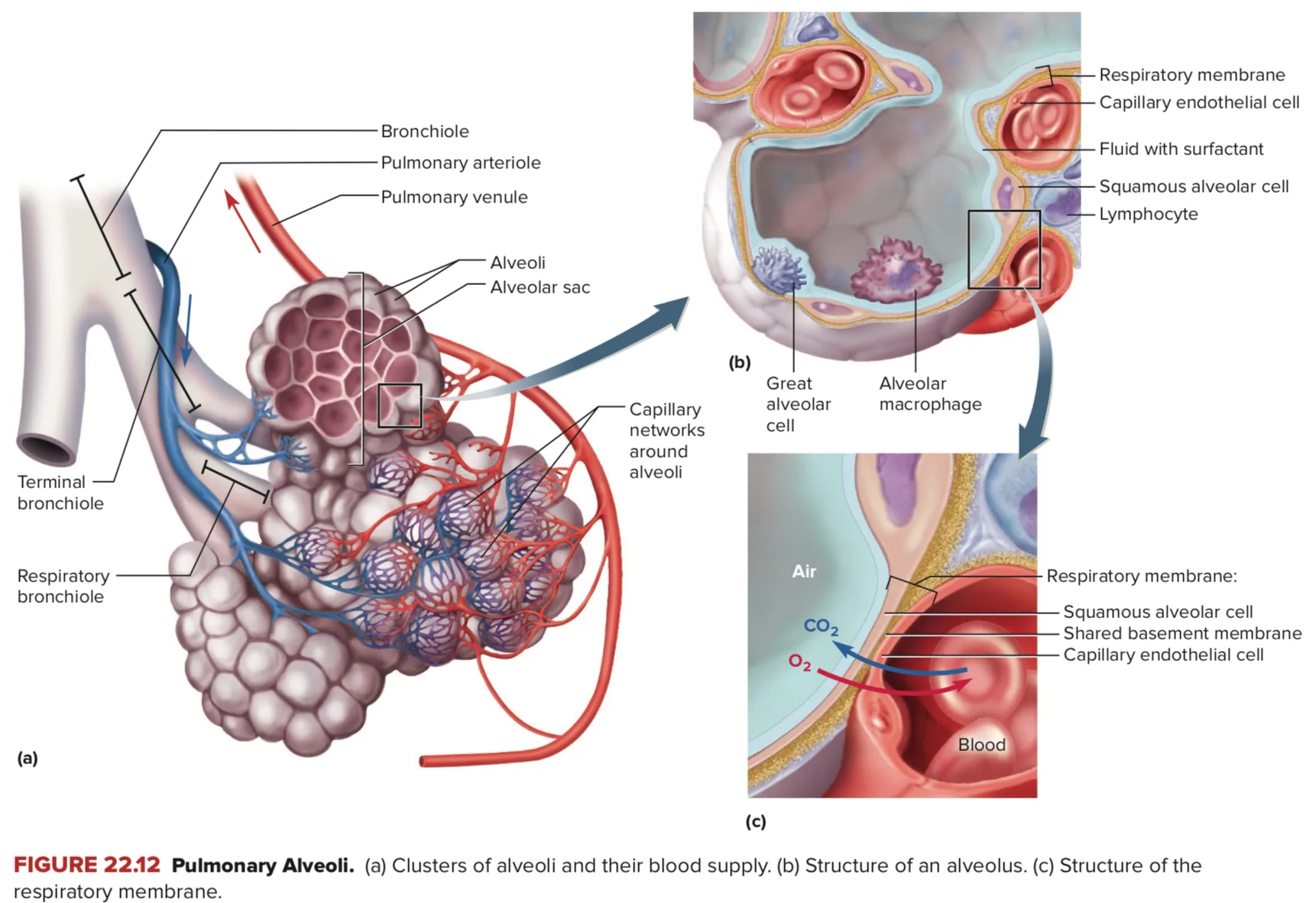
Capillary Network
- Proximity to Alveoli:
- Close Association: Pulmonary capillaries are tightly packed around alveoli.
- Capillary Wall Composition:
- Endothelial Cells: Extremely thin endothelial layers ensure minimal barriers for gas diffusion.
- Functional Advantage:
- Enhanced Gas Exchange: The close and thin arrangement between alveoli and capillaries promotes efficient transfer of gases.
Additional Cellular Components
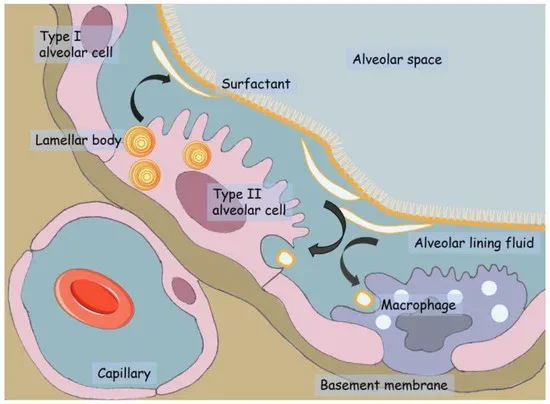
Type II Alveolar Cells
- Function:
- Surfactant Production: Secrete pulmonary surfactant, a substance that reduces surface tension within the alveoli, preventing collapse and ensuring alveoli remain open for gas exchange.
- Regeneration:
- Repair Role: Capable of dividing and differentiating to replace damaged Type I cells, aiding in alveolar repair and maintenance.
3. Gas Exchange Process in Alveoli
Mechanism of Gas Diffusion
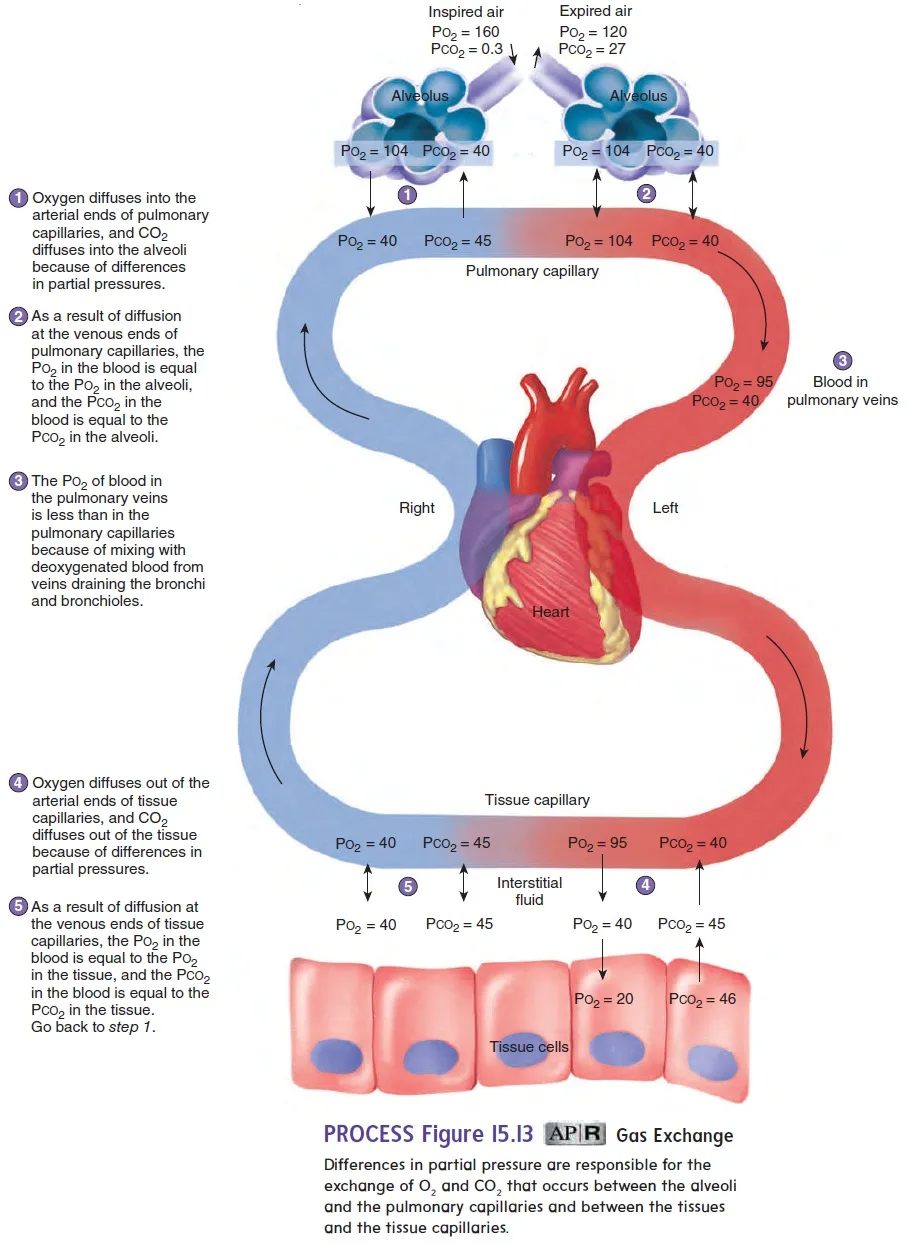
Oxygen (O₂) Diffusion
- Direction: From alveolar air (high O₂ concentration) to the blood in capillaries (low O₂ concentration).
- Process: Oxygen molecules pass through the alveolar and capillary walls to bind with hemoglobin in red blood cells.
Carbon Dioxide (CO₂) Diffusion
- Direction: From the blood in capillaries (high CO₂ concentration) to the alveolar air (low CO₂ concentration).
- Process: Carbon dioxide molecules pass through the alveolar and capillary walls to be exhaled out of the body.
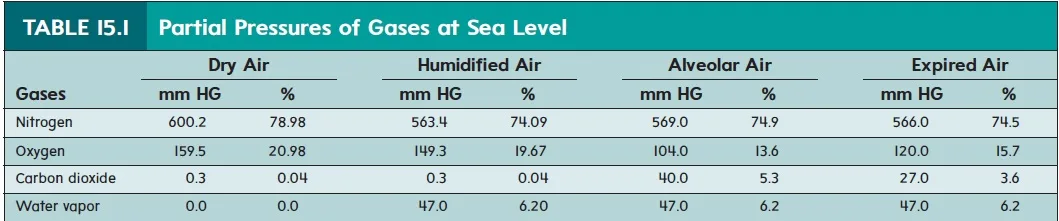
Concentration Gradients
- Importance: A steep concentration gradient is essential for the efficient diffusion of gases.
- Maintenance Mechanisms:
- Breathing (Ventilation): Continuously brings in fresh air with high O₂ and removes air with high CO₂.
- Blood Flow (Perfusion): Constant circulation of deoxygenated blood rich in CO₂ and low in O₂ ensures gradients are maintained for ongoing gas exchange.
Respiratory Membrane
- Composition:
- Layers: Consists of the alveolar epithelium, the capillary endothelium, and their fused basement membranes.
- Thickness: Approximately 0.5–1.0 μm in total.
- Function: Facilitates rapid gas exchange by minimizing the distance over which gases must diffuse.
Partial Pressures and Gas Exchange
- Partial Pressure of Oxygen (PO₂):
- Higher in alveolar air (~104 mmHg) compared to blood in pulmonary capillaries (~40 mmHg), driving O₂ into the blood.
- Partial Pressure of Carbon Dioxide (PCO₂):
- Higher in blood (~46 mmHg) compared to alveolar air (~40 mmHg), driving CO₂ out of the blood.
4. Key Terms
- Elastic Fibers:
- Protein fibers within alveolar walls that allow alveoli to stretch during inhalation and recoil during exhalation.
- Squamous Epithelium (Type I Alveolar Cells):
- A single layer of flat, thin cells lining the alveoli, minimizing the distance for gas diffusion.
- Endothelial Cells:
- Thin cells that line the capillaries surrounding alveoli, facilitating efficient gas exchange.
- Type II Alveolar Cells:
- Cells that produce surfactant and aid in the repair and maintenance of alveolar structures.
- Surfactant:
- A mixture of lipids and proteins secreted by Type II alveolar cells that reduces surface tension within the alveoli.
- Respiratory Membrane:
- The barrier through which gas exchange occurs, comprising the alveolar epithelium, capillary endothelium, and their fused basement membranes.
- Partial Pressure:
- The pressure exerted by an individual gas in a mixture of gases, crucial for driving diffusion during gas exchange.
5. Summary of Oxygen Pathway (From Atmosphere to Bloodstream)
- Inhalation Pathway:
- Air Entry: Inhaled through the nose or mouth.
- Pathway Sequence: Nose/Mouth → Trachea → Bronchi → Bronchioles → Alveolar Ducts → Alveoli.
- Diffusion Process:
- Across Alveolar Epithelium: Oxygen diffuses from alveolar air into the alveolar epithelial cells.
- Across Capillary Endothelium: Oxygen moves from epithelial cells into the blood within capillaries.
- Binding to Hemoglobin: Oxygen binds to hemoglobin molecules in red blood cells for transport throughout the body.
6. Adaptations of Alveoli for Gas Exchange
- Large Surface Area:
- The presence of millions of alveoli collectively provides an extensive surface area (~70–75 m²) to maximize gas exchange.
- Thin Walls:
- Alveolar and capillary walls consist of single cell layers, minimizing the distance for gas diffusion.
- Rich Blood Supply:
- Dense network of capillaries ensures a continuous supply of blood with appropriate concentration gradients for O₂ and CO₂.
- Elasticity:
- Elastic fibers allow alveoli to expand and contract efficiently, maintaining optimal surface area and ventilation.
- Surfactant Production:
- Reduces surface tension, preventing alveolar collapse and ensuring stability during breathing cycles.
7. Advantages of Bronchiole Diameter Adjustment
Smooth Muscle Control
- Functionality:
- Contraction: Narrows bronchiole diameter, reducing airflow when necessary (e.g., during rest).
- Relaxation: Widens bronchiole diameter to increase airflow, especially during increased physical demand like exercise.
Absence of Cartilage
- Flexibility:
- Without rigid cartilage, bronchioles can dynamically adjust their diameter, allowing precise regulation of airflow to different regions of the lungs based on the body’s needs.
8. Additional Concepts
Cell Membrane Crossings by Oxygen
- Pathway:
- Alveolar Epithelial Cell Membrane: Oxygen crosses both the inward and outward membranes.
- Capillary Endothelial Cell Membrane: Oxygen crosses both the inward and outward membranes.
- Red Blood Cell Membrane: Oxygen crosses the membrane to bind with hemoglobin.
- Total Membranes Crossed: Five membranes for oxygen to move from alveolar air to hemoglobin in red blood cells.
Bohr Effect
- Definition:
- The Bohr effect describes how increased CO₂ concentration and decreased pH in the blood facilitate the release of oxygen from hemoglobin.
- Physiological Relevance:
- Enhances oxygen delivery to tissues that are actively metabolizing and producing more CO₂.
Role of Surfactant
- Function:
- Surfactant reduces surface tension within alveoli, preventing collapse during exhalation and reducing the effort required to expand the lungs during inhalation.
- Clinical Relevance:
- Deficiency in surfactant production can lead to respiratory distress syndrome, particularly in premature infants.
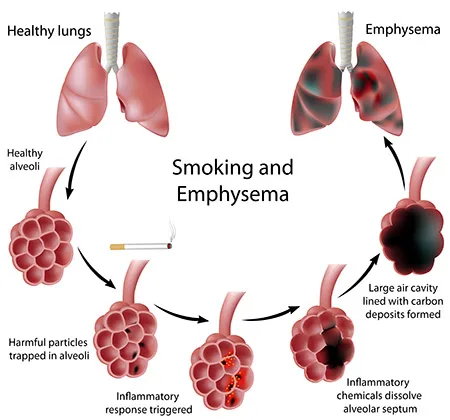
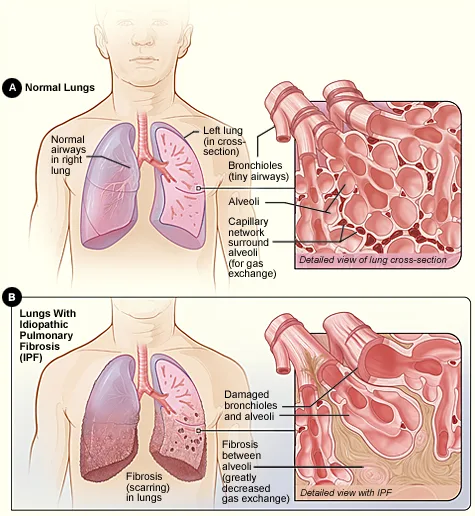
Common Alveolar Diseases
- Emphysema:
- A condition characterized by the destruction of alveolar walls, leading to reduced surface area for gas exchange and impaired respiratory function.
- Pulmonary Fibrosis:
- Involves the thickening and scarring of alveolar walls, hindering gas diffusion and causing breathing difficulties.