11.01 Antibodies & Blood Groups
Antibody Basics
Antibodies (Immunoglobulins):
- Definition: Glycoproteins produced by B lymphocytes (a type of white blood cell) that specifically recognize and bind to antigens.
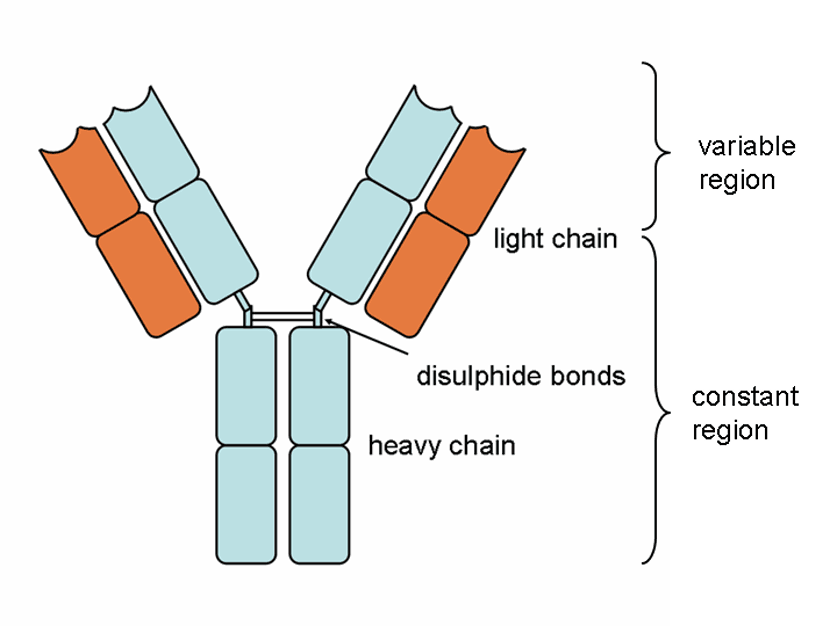
- Structure: Typically Y-shaped molecules composed of four polypeptide chains (two heavy and two light chains) with variable regions that determine antigen specificity.
- Function:
- Recognition: Bind to specific epitopes on antigens, marking them for destruction.
- Neutralization: Prevent pathogens or toxins from interacting with host cells.
- Opsonization: Enhance phagocytosis by tagging antigens for immune cells.
- Complement Activation: Initiate the complement cascade, leading to the lysis of pathogens.
Structure of Antibodies
- Specificity: The unique sequence of amino acids in the variable region creates a specific three-dimensional shape tailored to bind a particular antigen. This specificity is achieved through interactions between the antigen and the antibody’s R groups (side chains).
Basic Composition
- Globular Glycoproteins: Antibodies are globular (spherical) proteins with attached carbohydrate groups, making them glycoproteins.
- Quaternary Structure: They possess a quaternary structure, meaning they are composed of multiple polypeptide chains assembled together.
Polypeptide Chains
- Heavy Chains: Each antibody has two identical heavy chains.
- Light Chains: Each antibody also has two identical light chains.
- Disulfide Bridges: The heavy and light chains are interconnected by disulfide bonds, stabilizing the overall structure.
Y-Shaped Structure
- Overall Shape: The assembly of these chains forms a characteristic Y-shaped molecule.
- Regions of the Y-Shape:
- Constant Region (Lower Part of the Y):
- Uniformity: This region has a consistent amino acid sequence across all antibodies of the same class.
- Function: It binds to receptors on immune cells like phagocytes, macrophages, and neutrophils.
- Class Determination: The constant region defines the class of the antibody (e.g., IgM, IgG, IgA, IgE).
- Variable Region (Upper Part of the Y):
- Diversity: This region varies among different antibodies, allowing for the specific recognition of diverse antigens.
- Binding Sites: Each antibody has two identical binding sites within the variable region, formed by both light and heavy chains.
- Constant Region (Lower Part of the Y):
Antibody Mechanisms
- Viral Inhibition: Antibodies prevent viruses from binding to or damaging host cells.
- Reduced Bacterial Mobility: Antibodies bind to bacterial flagella, limiting movement and aiding phagocytosis.
- Agglutination: Causes clumping of bacteria, reducing their spread.
- Bacterial Lysis: Some antibodies create pores in bacterial cell walls, leading to cell burst due to osmotic pressure.
- Enhanced Phagocytosis: Antibodies coat pathogens, making them easier for phagocytes to ingest via receptor binding.
- Antitoxin Action: Specialized antibodies (antitoxins) neutralize bacterial toxins.
Immune Responses and Immunological Memory
- Secondary Immune Response: Faster, stronger response due to memory B cells. Leads to rapid antibody production and higher antibody levels, often preventing symptoms.
- Primary Immune Response: Initial response to a specific antigen; slow due to low specific B cell count.
Cell Surface Antigens
Definition:
- Cell Surface Antigens: Molecules present on the surface of cells that are unique to each individual or organism. They include proteins and carbohydrates that serve as markers distinguishing self from non-self.
Role in Immunity:
- Self vs. Non-Self Recognition:
- Self Antigens: Recognized by the immune system as part of the body, preventing an immune response.
- Non-Self Antigens: Recognized as foreign, triggering an immune response.
- Immune Tolerance: The immune system does not typically produce antibodies against self antigens, avoiding autoimmunity.
- Cross-Reactivity: When antigens from another individual (e.g., in blood transfusion) are introduced, they can trigger an immune response.
Example: ABO Blood Group Antigens
- ABO System: Determines blood types based on the presence of specific carbohydrate antigens on red blood cells (RBCs).
- Blood Group A: Possesses the A antigen (a specific carbohydrate structure) on RBCs.
- Blood Group B: Possesses the B antigen.
- Blood Group AB: Possesses both A and B antigens.
- Blood Group O: Possesses neither A nor B antigens.

ABO Blood Group System
Blood Group A:
- Antigens: Contains A-specific carbohydrate chains attached to glycolipids and glycoproteins on RBC surfaces.
- Antibodies: Naturally occurring anti-B antibodies in the plasma.
Immune Reaction in Blood Transfusion:
- Incorrect Transfusion Example:
- Scenario: Transfusing blood group A to a blood group B recipient.
- Immune Response: The recipient’s anti-A antibodies recognize the A antigens on the transfused RBCs as foreign, leading to agglutination (clumping) and hemolysis (destruction) of RBCs.
- Correct Transfusion Example:
- Scenario: Transfusing blood group B to a blood group B recipient.
- Outcome: The recipient’s immune system recognizes the B antigens as self, preventing an immune reaction.
Why Type B Blood Isn’t Given to Type A Individuals:
- Reason: Blood group A individuals possess anti-B antibodies. Introducing type B blood would result in these antibodies attacking the foreign B antigens, causing an immune rejection.

Immune Response Overview
Lymphocytes’ Role:
- B Lymphocytes (B Cells):
- Function: Produce antibodies specific to antigens encountered.
- Activation: Require antigen binding and helper T cell signals for activation and differentiation into plasma cells.
- T Lymphocytes (T Cells):
- Helper T Cells (CD4+): Assist in activating B cells and other immune cells.
- Cytotoxic T Cells (CD8+): Directly kill infected or cancerous cells presenting foreign antigens.
Immune Mechanisms:
- Humoral Immunity: Mediated by antibodies produced by B cells, targeting extracellular pathogens and toxins.
- Cell-Mediated Immunity: Involves T cells targeting infected cells and coordinating the immune response.
Differences Between Antibodies and Antibiotics
| Feature | Antibodies | Antibiotics |
|---|---|---|
| Origin | Produced by the immune system (B cells) | Synthetic or natural drugs manufactured by humans |
| Function | Target specific antigens (proteins, pathogens) | Kill or inhibit the growth of bacteria |
| Specificity | Highly specific to particular antigens | Broad or narrow spectrum depending on the type |
| Mechanism | Bind to antigens, neutralize pathogens, facilitate phagocytosis | Disrupt bacterial cell walls, protein synthesis, DNA replication, etc. |
| Usage | Part of natural immune response, used in therapies like monoclonal antibodies | Used as medications to treat bacterial infections |
Self vs. Non-Self Recognition in the ABO System
Mechanism:
- Self Recognition:
- The immune system identifies its own cell surface antigens (e.g., A or B antigens) as self.
- Prevents the production of antibodies against these antigens.
- Non-Self Recognition:
- Introduction of foreign antigens (e.g., from a different blood type) is recognized as non-self.
- Triggers the production of specific antibodies against these antigens.
Example:
- Blood Group A Individuals:
- Self Antigen: A antigen on their RBCs.
- Non-Self Antigen: B antigen from another blood type.
- Immune Response: Presence of anti-B antibodies that react against B antigens.
Key Terms
- Antibody (Immunoglobulin): A glycoprotein produced by B lymphocytes that specifically binds to an antigen.
- Antigen: A molecule capable of inducing an immune response, typically a protein or polysaccharide on pathogens.
- Lymphocytes: White blood cells involved in the adaptive immune response, including B cells and T cells.
- Humoral Immunity: Immune response mediated by antibodies in body fluids.
- Cell-Mediated Immunity: Immune response involving T cells that target infected or abnormal cells.
- Phagocytes: Immune cells (e.g., macrophages, neutrophils) that engulf and digest pathogens and debris.
- Agglutination: Clumping of cells (e.g., RBCs) caused by antibodies binding to antigens.
- Hemolysis: Destruction of red blood cells, often resulting from an immune reaction.
- Opsonization: Process by which antibodies mark pathogens for ingestion and destruction by phagocytes.
- Complement System: A group of proteins that assists antibodies in clearing pathogens through lysis, opsonization, and inflammation.
Additional Notes:
Monoclonal vs. Polyclonal Antibodies:
- Monoclonal Antibodies: Identical antibodies produced by a single B cell clone, specific to one epitope.
- Polyclonal Antibodies: A mixture of antibodies produced by different B cell clones, targeting multiple epitopes on the same antigen.
Antibody Structure and Classes:
- IgG: Most abundant, provides long-term immunity, crosses the placenta.
- IgM: First antibody produced in response to an infection.
- IgA: Found in mucosal areas, such as the gut, respiratory tract, and saliva.
- IgE: Involved in allergic reactions and defense against parasites.
- IgD: Functions mainly as a receptor on B cells.
Blood Transfusion Compatibility:
- Importance of cross-matching blood before transfusion to ensure compatibility.
- Understanding of Rh factor (positive/negative) in addition to ABO blood group.
Immune System Disorders:
- Autoimmune Diseases: Result from the immune system mistakenly targeting self-antigens.
- Immunodeficiencies: Conditions where the immune system is less effective, increasing susceptibility to infections.